Key takeaways:
- IPMN is an acronym for intraductal papillary mucinous neoplasms of the pancreas. It is also known as a pancreatic cystic neoplasm.
- Pancreatic cysts are typically found when patients undergo abdominal imaging for other reasons.
- An IPMN is a benign (non-cancerous), fluid-filled pancreatic cyst.
- Though IPMN cysts are benign, they can develop into malignant tumours. This type of pancreatic cancer can become an invasive cancer that is difficult to treat1.
Being diagnosed with IPMNs often comes as a surprise, as they are usually discovered during a screening for something unrelated to the pancreas.
The diagnosis of an IPMN may feel overwhelming. However, pancreatic cysts associated with IPMN don’t always turn into pancreatic cancer. In fact, the prevalence of pancreatic cancer associated with IPMN is relatively low2.
Early detection and diagnosis can lead to effective treatment that offsets the risk of malignancy. Increased awareness of invasive IPMN has enabled pancreatectomies (surgical removal of the pancreas) to be performed at an earlier stage, similar to common pancreatic cancer.
What Are IPMNs?
Intraductal papillary mucinous neoplasms of the pancreas (IPMN) are cysts or fluid-filled sacs found in the pancreas.
These types of cysts are benign, which means they are not cancerous. However, in 1 to 11 per cent of patients, an IPMN can be aggressive. Aggressive IPMN can develop into pancreatic ductal adenocarcinoma, a lethal form of pancreatic cancer3.
Even though they’re benign, you shouldn’t ignore IPMN. Schedule and attend follow-up appointments as recommended by your medical practitioner.
About the Pancreas
The pancreas is an organ in the abdomen that is located behind the stomach and directly connected to other major organs in the digestive tract.
As a key part of the digestive system, the pancreas produces hormones that regulate various bodily functions and digestive enzymes that help the body process food.
There are four main parts of the pancreas:
- The head of the pancreas
- The neck of the pancreas
- The body of the pancreas
- The tail of the pancreas
The pancreas has a main duct, sometimes referred to as the main pancreatic duct, which has several branches. The digestive enzymes produced by your pancreas move through the branches, into the main duct, and into the small intestine.
As previously mentioned, the pancreas also produces essential hormones vital to many digestive and metabolic processes. Some of these hormones include insulin and glucagon. Both are important for regulating your blood sugar levels4.
Key Acronyms Related to IPMN
In addition to IPMN itself, there are many other acronyms associated with IPMN5,6. Use this list as a handy reference whenever these terms come up during your appointments:
Types of Cysts, Tumours, and Lesions That Affect the Pancreas
A cyst is a formation of cells that forms a sac. The sac may be filled with fluid, air, or solid material. Tumours are groups of cells growing abnormally, forming lumps or growths. Lesions are areas of abnormal or damaged tissue.
There are various types of pancreatic cysts, tumours, and lesions:
- Cystic lesions: a broad group of pancreatic abnormalities that have a cystic (fluid-like) appearance. They can be benign or malignant.
- Cystic neoplasms: one or more fluid-filled sacs (cysts) arising from tumour (neoplastic) cells.
- Pancreatic cystic tumours: tumours in the pancreas containing fluid that could be either serous (watery-like fluid) or mucinous (mucus-like fluid).
An IPMN is a mucinous cyst characterised by its viscous fluid. IPMNs develop inside the main pancreatic duct and its branches. Some IPMNs reach out into the pancreatic duct system or branches of the duct. These are called branch duct IPMN.
All types of pancreatic cysts are typically found when patients receive abdominal imaging for other reasons. For example, a radiologist could see a pancreatic cyst when they’re looking at a gastric ulcer.
As we age, we are more susceptible to pancreatic cysts. The occurrence of pancreatic cysts is 17 per cent in those aged 30-39 and 76 per cent in those aged over 80 years7. Better access to diagnostic tools such as MRI scans could lead to more cysts being discovered earlier8.
Risk Factors for IPMN
IPMN formation is strongly age-driven. Smoking, excess alcohol consumption, and severe obesity (BMI exceeding 35) can all increase the risk of IPMN turning into pancreatic cancer1.
Signs and Symptoms of IPMN
Usually, people are unaware that they have an IPMN because there aren’t any signs or symptoms.
Sometimes, people with an IPMN will develop acute pancreatitis, and the uncomfortable symptoms may prompt them to see their medical provider.
Similar symptoms could be caused by many conditions, so it might be hard to connect them to IPMNs1. These include:
- Jaundice (yellow eyes or skin)
- Fatigue
- Appetite loss or unexplained weight loss
- Pain in the tummy (abdomen)
- Stomach upset, nausea, vomiting, constipation, and diarrhoea
Types of IPMNs That May Affect Your Pancreas
IPMNs are usually put into one of two categories:
- IPMNs associated with invasive cancer.
- IPMNs where there is no invasive cancer present
IPMNs with no associated invasive cancer are placed into one of two subtypes:
- Low-grade dysplasia (LGD)
- High-grade dysplasia (HGD)
Dysplasia means the cell’s state is abnormal. In some cases, this might mean that the cell is pre-cancerous.
Over time, IPMNs may progress from low-grade to high-grade dysplasia. In the case of HGD, the disease may progress to invasive pancreatic cancer.
IPMNs are further evaluated and classified according to their location in the pancreas:
- Main duct
- Branch duct
- Both the main duct and the branch duct
IPMNs need to be classified to help make decisions around treatment9.
How Your Medical Practitioner Looks for or Treats an IPMN
Many tests can help look for and monitor an IPMN once it’s found. Usually, observation is the only action taken for IPMNs. They are most often not considered to be at high risk for developing cancer.
1. Abdominal Ultrasound
This non-intrusive screening test can reveal a narrowing within the common bile duct, which is a marker of IPMN.
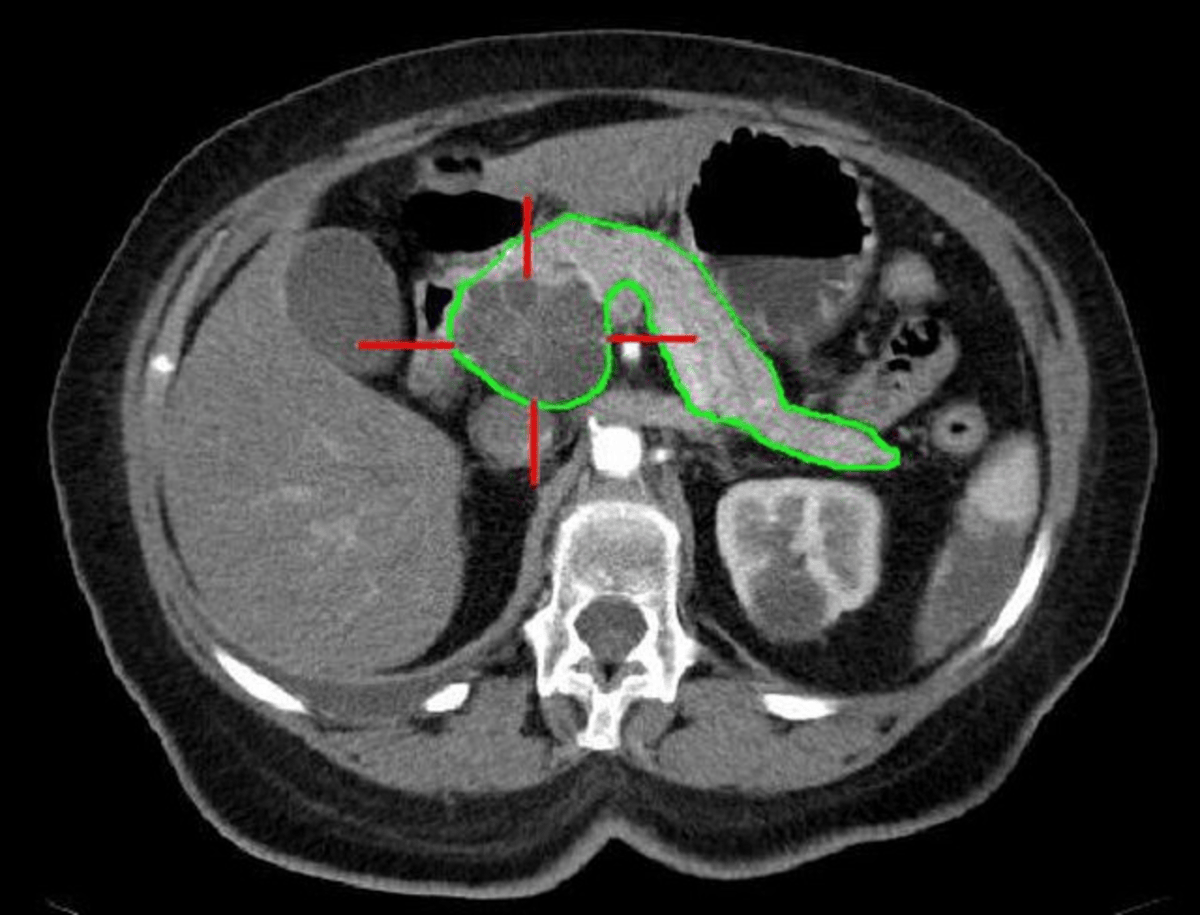
2. Abdominal Computed Tomography (CT Scan) or MRI
A CT scan or abdominal MRI can identify narrowing within the biliary tract. Both scans are noninvasive procedures, during which the bile duct images are shown on a computer monitor.
3. Laparoscopy
A small surgical operation, also known as keyhole surgery. Surgery may be recommended in high-risk cases where the location of the IPMN allows it to be easily removed1,6.
IPMNs of the main duct might be candidates for surgery more often than those found only in the branches. This is because IPMNs within the ductal branches are more difficult to treat and are less aggressive than main duct IPMNs10.
Treatment Options for Pancreatic Cancer
If invasive IPMN has evolved into cancer, treatment is undertaken to remove part of the pancreas or, rarely, the entire pancreas.
There are three common types of pancreatic surgery to treat pancreatic cancer:
1. Distal pancreatectomy
This surgery removes a section from the pancreas body (middle) and from the tail of the pancreas, which is the part of the pancreas that is closest to the spleen. In some cases, your surgeon might also remove the spleen.
Usually, enough of the pancreas is left that pancreatic function will not be affected.
2. Pancreaticoduodenectomy
Also called Whipple’s operation, this surgery removes the head of the pancreas. Sometimes, the part of the small intestine, part of the bile duct, the gallbladder, and part of the stomach are removed as well.
3. Total pancreatectomy
This is the procedure to remove the entire pancreas. Likewise, your surgical team will also remove the spleen, part of the stomach, gallbladder and part of the bile duct, and a portion of the small intestine.
If the whole pancreas is removed, the stomach will need to be connected to the remaining section of the small intestine for digestion11.
Early Detection Is Key to Detecting IPMN and Preventing Cancer
The pancreas is responsible for essential body functions related to our digestive and hormone regulation. An IPMN is one of several conditions that could happen to your pancreas.
IPMN causes pancreatic inflammation or pancreatitis. When this occurs, the cells that line our pancreatic duct can become premalignant. In other words, there is a chance these cells could spiral into pancreatic cancer, a notoriously difficult type of cancer to treat.
Most often, pancreatic cysts are not cancerous and can be readily managed, preventing cancer.
If you want to be proactive about your health, why not consider an Ezra MRI scan? Our MRI scans for hundreds of conditions, including cancers of the pancreas. Book your appointment with us today.
Understand your risk for cancer with our 5 minute quiz.
Our scan is designed to detect potential cancer early.
References
1. NHS. Pancreatic cysts - intraductal papillary mucinous neoplasm. Guy’s and St Thomas’ NHS Foundation Trust. November 2022. Accessed December 8, 2025. https://www.guysandstthomas.nhs.uk/health-information/pancreatic-cysts-intraductal-papillary-mucinous-neoplasm
2. Lucocq J, Pandanaboyana S. Pancreatic cancer arising in intraductal papillary mucinous neoplasms (IPMN): emerging data warrants further research. BJS. 2024;111(10):znae238. doi:10.1093/bjs/znae238
3. Del Chiaro M, Ateeb Z, Hansson MR, et al. Survival analysis and risk for progression of intraductal papillary mucinous neoplasia of the pancreas (IPMN) under surveillance: a single-institution experience. Ann Surg Oncol. 2017;24(4):1120-1126. doi:10.1245/s10434-016-5661-x
4. NHS. What is the pancreas? Leeds Teaching Hospitals NHS Trust. March 7, 2024. Accessed December 8, 2025. https://www.leedsth.nhs.uk/services/pancreas-unit/what-is-the-pancreas/
5. Cancer Research UK. Tests for pancreatic cancer. Cancer Research UK. May 2023. Accessed December 8, 2025. https://www.cancerresearchuk.org/about-cancer/pancreatic-cancer/getting-diagnosed/tests-pancreatic-cancer
6. Pancreatic Cancer UK. Pancreatic cysts. Pancreatic Cancer UK. December 2025. Accessed December 8, 2025. https://www.pancreaticcancer.org.uk/information/just-diagnosed-with-pancreatic-cancer/pancreatic-cysts/
7. Kromrey ML, Bülow R, Hübner J, et al. Prospective study on the incidence, prevalence and 5-year pancreatic-related mortality of pancreatic cysts in a population-based study. Published online January 1, 2018. doi:10.1136/gutjnl-2016-313127
8. Shah S, Muthusamy VR. Pancreatic cystic lesions in the older patient: a review of clinical guidelines and management. Curr Gastroenterol Rep. 2025;27(1):72. doi:10.1007/s11894-025-01004-3
9. The European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67(5):789-804. doi:10.1136/gutjnl-2018-316027
10. Dal Borgo C, Perri G, Borin A, Marchegiani G, Salvia R, Bassi C. The Clinical Management of Main Duct Intraductal Papillary Mucinous Neoplasm of the Pancreas. Dig Surg. 2018;36(2):104-110. doi:10.1159/000486869
11. Pancreatic Cancer UK. Surgery to remove pancreatic cancer. Pancreatic Cancer UK. October 2023. Accessed December 9, 2025. https://shop.pancreaticcancer.org.uk/products/surgery-to-remove-pancreatic-cancer