When it comes to your health, quality matters more than quantity; better data beats more data every time. For a truly effective full-body MOT, start with these six essential tests. Focus on their results, take action where needed, and ignore the rest of the noise. Your health deserves clarity, not clutter.
Test 1 - Full-Body MRI Baseline Analysis
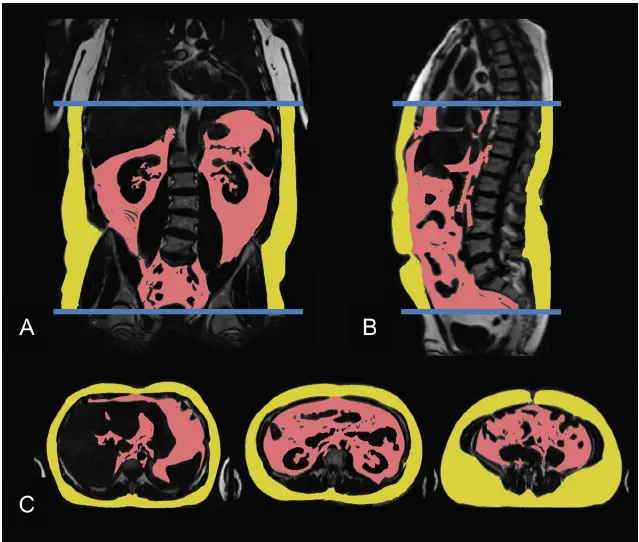
A full-body MRI is the smartest first step in your health MOT. This scan provides a clear and detailed view of your body, allowing you to spot tumours, measure hidden visceral fat, and detect organ inflammation before symptoms appear.
This also provides a baseline for reference. Furthermore, MRI does not use ionising radiation, making it safer than other screening processes, especially for pediatric patients and those requiring repeated imaging1.
Why Start Here?
This test quantifies hidden risks that other checkups might miss. It measures visceral fat, a major driver of chronic disease, and can also detect potential cancers and abnormalities1,2. By catching problems early, you increase your chances of preventing serious health issues before they develop.
Why Is It So Important?
Studies have found that a visceral adipose tissue (VAT) area above 110 cm2 is associated with a significantly higher frequency of insulin resistance, while a VAT of 106-162 cm2 increases the risk of impaired glucose tolerance3,4.
Even with a normal BMI, high visceral fat signals elevated risk due to its inflammatory effects. For example, higher visceral adipose tissue is associated with a 48% increased risk of breast cancer even among normal-weight postmenopausal women5.
What Can I Do to Reduce My Risk?
To lower visceral fat and improve your scan results, consider prioritising a diet rich in whole foods, regular strength training, and consistent aerobic exercise6. You can keep track of your progress by retesting with another full-body MRI in 12-18 months.
Ezra’s full-body MRI utilises advanced imaging and AI to screen for over 500 conditions across 13 organs, providing an accessible and proactive approach to detecting signs of early cancer and disease. Take Ezra’s 5-minute quiz to calculate your risk.
Test 2: Coronary Artery Calcium (CAC) Score
A coronary artery calcium (CAC) score uses a quick, non-invasive CT scan to measure the amount of calcified plaque in your heart’s arteries7. This test is now considered the gold standard for predicting future heart disease risk, as it directly visualises hardened plaque that can lead to heart attacks.
Why is CAC the Gold Standard?
CAC scoring is considered the gold standard for assessing cardiovascular risk because it directly measures the amount of calcified plaque in the coronary arteries, which is a highly specific marker of atherosclerosis. Large, long-term studies have shown that CAC scoring predicts the risk of major cardiovascular events more accurately than traditional risk factors alone8,9.
What Do Your CAC Results Mean?
- Score of 0: Very low risk for heart attack in the next five years10.
- Score above 0-100: Indicates the presence of plaque. Focus on lowering apolipoprotein B (ApoB), blood pressure, and inflammation to slow progression.
- Score over 100: Signals higher risk - intensify prevention efforts and consider more frequent monitoring.
If your CAC score is zero, it is recommended that you retake the test every five years11. If your score is over 100, you should rescan every two to three years to track changes and adjust your prevention plan as needed.
Test 3: Advanced Lipids & LDL Subfraction Analysis
Advanced lipid testing goes beyond basic cholesterol checks to uncover hidden heart risks. Think of it like this: a standard LDL test tells you how much ‘bad’ cholesterol is floating in your blood, like counting cargo boxes on ships.
But advanced testing shows you how many ‘ships’ (particles) there are and how dangerous they are. Small, dense particles slip easily into artery walls and cause plaque buildup, while larger particles are bulky and pass by harmlessly12.
ApoB vs. LDL-C: Why Particle Count Matters
ApoB directly measures the number of atherogenic particles. Each very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and low-density lipoprotein (LDL) particle carries one ApoB molecule13.
Research has shown that ApoB is a superior predictor of cardiovascular events compared to LDL-C14. When LDL-C and ApoB levels disagree (e.g., normal LDL-C but high ApoB), risk typically follows ApoB. Target levels of ApoB are <80 mg/dL15.
LDL Particle Size: Pattern A vs. Pattern B
LDL particle size patterns are generally categorised into two main types: Pattern A and Pattern B16.
- Pattern A: Large, buoyant LDL particles. Lower cardiovascular risk, even with elevated LDL-C.
- Pattern B: Small, dense LDL particles. Associated with 3-5x higher heart attack risk, insulin resistance, and low HDL. Small, dense LDL particles independently predict CAC and stroke.
The High-LDL Caveat: Context Matters
Elevated LDL-C isn’t uniformly dangerous. Lean Mass Hyper-responders (LMHRs), often fit, low-carb individuals, may exhibit LDL levels above 200 mg/dL, accompanied by high HDL levels (>80 mg/dL) and low triglyceride levels (<70 mg/dL)17.
This profile may reflect a process known as adaptive lipid metabolism, but the long-term risk remains unclear. LDL-C data should be paired with advanced testing to assess particle size and ApoB.
Remnant Cholesterol: The Triglyceride Threat
Remnant cholesterol (from triglyceride-rich lipoproteins like VLDL) is causally linked to cardiovascular disease and type 2 diabetes18. Each 1.0 mmol/L increase in triglycerides raises cardiometabolic risk by 26%. Keep fasting triglycerides <1.2 mmol/L (90 mg/dL) to minimise remnants19.
Lipid Optimisation Targets
Below, we have summarised the key targets for optimal lipid health. These numbers focus not just on cholesterol levels but also on the quality and quantity of lipid particles in the blood.
Test 4 - Insulin Resistance Panel
An insulin resistance panel assesses how effectively your body regulates blood sugar by measuring several key markers:
- Fasting Insulin: Shows how much insulin your body needs to keep blood sugar stable after not eating. The recommended reference values for fasting insulin in healthy adults generally range from 15.6 to 150 pmol/L23. NHS reference intervals for healthy men and women have an upper limit of <72 pmol/L24. However, in the coming years, it is possible that newer research will narrow this range.
- Fasting Glucose: Measures your blood sugar after fasting. High levels can be an early sign that your body isn’t handling sugar well25.
- Haemoglobin A1c (HbA1c): Reflects your average blood sugar over the past 2-3 months26. It helps spot long-term trends, not just daily changes.
- Homeostatic Model Assessment for Insulin Resistance (HOMA-IR): Combines your fasting insulin and glucose to estimate how resistant your body is to insulin27. Lower scores mean better insulin sensitivity.
Tracking these markers together helps identify early signs of metabolic problems, even before your blood sugar levels start to rise.
Why Insulin Resistance Matters
When your cells become resistant to insulin, your body must produce more of it to maintain normal blood sugar levels. Over time, this can lead to weight gain, increased blood sugar, and eventually type 2 diabetes or heart disease28.
If your results show rising insulin or HOMA-IR, focus on lifestyle changes, such as increasing fibre intake, reducing excess calories, and staying active, to improve your insulin sensitivity29,30. Early detection and action can also help you avoid serious problems down the line.
Test 5 - High-Sensitivity C-Reactive Protein
High-sensitivity C-reactive protein (hs-CRP) is a simple blood test that measures the overall level of inflammation in your body. CRP is a protein made by your liver, and its levels increase when there’s inflammation, even if you feel fine31. This test is sensitive enough to detect small increases that can signal hidden risks, especially for heart disease.
Why it's Important to Keep your hs-CRP Low
Keeping your hs-CRP below 2 mg/L is ideal and linked to the lowest risk for heart attacks and other cardiovascular problems32. Higher levels indicate that your body is experiencing more inflammation, which can be triggered by infections, poor lifestyle habits, or chronic diseases.
Test 6 - VO2max Stress Test
VO2max is the ultimate measure of your cardiorespiratory fitness, essentially, how efficiently your body uses oxygen during intense exercise33. Higher VO2max scores are strongly linked to longer, healthier lives, making this test a powerful predictor of mortality risk. Aim for the top quartile of your age group; for a healthy 40-year-old, that’s roughly 45 mL/kg/min34.
NHS Midlife Health Check: Good Floor, Not Enough Ceiling
The NHS Midlife Health Check offers a free basic assessment for adults aged 40-74, covering blood pressure, cholesterol, blood sugar, BMI, and lifestyle factors35. It’s a solid baseline for identifying common risks, such as heart disease and diabetes.
However, it doesn’t include advanced tests such as full-body MRI, CAC scoring, or VO2 max. Stacking this six-test MOT on top of the NHS check gives you deeper, more actionable insights into your long-term health.
12-Month Health Upgrade Roadmap
Q1: Establish your baseline with a full-body MRI, CAC score, and comprehensive lab panel.
Q2: Begin exercising and retest your VO2max to track cardiorespiratory improvements.
Q3: Focus on tightening up your lipid profile and lowering inflammation (CRP) with diet and exercise.
Q4: Re-check key markers like ApoB and HOMA-IR, then adjust your plan based on results.
Summary: Midlife Health Audit
You don’t need a 200-line lab spreadsheet to understand your health. Cut through the noise and focus on the data that truly moves the risk dial. With these six targeted tests, you’ll get clear, actionable insights: no guesswork required.
If you or your family wants to be proactive about your brain health, why not book an Ezra full-body MRI? Our annual scan catches potential cancer earlier, leveraging artificial intelligence through the screening process to make it more efficient, affordable, and faster.
Understand your risk for cancer with our 5 minute quiz.
Our scan is designed to detect potential cancer early.
References
1. Hochhegger B. Whole-body magnetic resonance imaging: an effective and underutilized technique. Radiol Bras. 2015;48(3):IX-X. doi:10.1590/0100-3984.2015.48.3e3
2. Crabtree CD, LaFountain RA, Hyde PN, et al. Quantification of Human Central Adipose Tissue Depots: An Anatomically Matched Comparison Between DXA and MRI. Tomography. 2019;5(4):358-366. doi:10.18383/j.tom.2019.00018
3. Salihefendic D, Zildzic M, Masic I. The Importance of the Quantity and the Distribution Assessment of Fat Tissue in a Diagnosis of Insulin Resistance. Med Arch. 2020;74(6):439-443. doi:10.5455/medarh.2020.74.439-446
4. Nicklas BJ, Penninx BWJH, Ryan AS, et al. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care. 2003;26(5):1413-1420. doi:10.2337/diacare.26.5.1413
5. Bea JW, Ochs-Balcom HM, Valencia CI, et al. Abdominal visceral and subcutaneous adipose tissue associations with postmenopausal breast cancer incidence. JNCI Cancer Spectr. 2025;9(1):pkaf007. doi:10.1093/jncics/pkaf007
6. Zając-Gawlak I, Kłapcińska B, Kroemeke A, et al. Associations of visceral fat area and physical activity levels with the risk of metabolic syndrome in postmenopausal women. Biogerontology. 2017;18(3):357-366. doi:10.1007/s10522-017-9693-9
7. Pathakota SR, Durgaprasad R, Velam V, et al. Correlation of coronary artery calcium score and carotid artery intima-media thickness with severity of coronary artery disease. J Cardiovasc Thorac Res. 2020;12(2):78-83. doi:10.34172/jcvtr.2020.14
8. Hisamatsu T, Kinuta M. Coronary Artery Calcium in Assessment of Atherosclerotic Cardiovascular Disease Risk and its Role in Primary Prevention. J Atheroscler Thromb. 2023;30(10):1289-1302. doi:10.5551/jat.RV22009
9. Greenland P, Blaha MJ, Budoff MJ, et al. Coronary Calcium Score and Cardiovascular Risk. JACC. 2018;72(4):434-447. doi:10.1016/j.jacc.2018.05.027
10. Shin JM, Kim TH, Kim JY, et al. Coronary artery calcium scoring on non-gated, non-contrast chest computed tomography (CT) using wide-detector, high-pitch and fast gantry rotation: comparison with dedicated calcium scoring CT. J Thorac Dis. 2020;12(10):5783-5793. doi:10.21037/jtd-20-1371
11. Golub IS, Termeie OG, Kristo S, et al. Major Global Coronary Artery Calcium Guidelines. JACC: Cardiovascular Imaging. 2023;16(1):98-117. doi:10.1016/j.jcmg.2022.06.018
12. Jin X, Yang S, Lu J, et al. Small, Dense Low-Density Lipoprotein-Cholesterol and Atherosclerosis: Relationship and Therapeutic Strategies. Front Cardiovasc Med. 2022;8:804214. doi:10.3389/fcvm.2021.804214
13. Behbodikhah J, Ahmed S, Elyasi A, et al. Apolipoprotein B and Cardiovascular Disease: Biomarker and Potential Therapeutic Target. Metabolites. 2021;11(10):690. doi:10.3390/metabo11100690
14. Benn M, Nordestgaard BG, Jensen GB, et al. Improving prediction of ischemic cardiovascular disease in the general population using apolipoprotein B: the Copenhagen City Heart Study. Arterioscler Thromb Vasc Biol. 2007;27(3):661-670. doi:10.1161/01.ATV.0000255580.73689.8e
15. Briers PJ, Langlois MR. Concordance of apolipoprotein B concentration with the Friedewald, Martin-Hopkins, and Sampson formulas for calculating LDL cholesterol. Biochem Med (Zagreb). 2022;32(1):010704. doi:10.11613/BM.2022.010704
16. Austin MA, King MC, Vranizan KM, et al. Inheritance of low-density lipoprotein subclass patterns: results of complex segregation analysis. Am J Hum Genet. 1988;43(6):838-846.
17. Norwitz NG, Soto-Mota A, Feldman D, et al. Case Report: Hypercholesterolemia “Lean Mass Hyper-Responder” Phenotype Presents in the Context of a Low Saturated Fat Carbohydrate-Restricted Diet. Front Endocrinol (Lausanne). 2022;13:830325. doi:10.3389/fendo.2022.830325
18. Zhao Y, Zhuang Z, Li Y, et al. Elevated blood remnant cholesterol and triglycerides are causally related to the risks of cardiometabolic multimorbidity. Nat Commun. 2024;15(1):2451. doi:10.1038/s41467-024-46686-x
19. Xie Y, Guo L, Chen H, et al. Determination of the postprandial cut-off value of triglyceride after a daily meal corresponding to fasting optimal triglyceride level in Chinese subjects. Front Nutr. 2023;10. doi:10.3389/fnut.2023.1037270
20. Rosenson RS, Underberg JA. Systematic Review: Evaluating the Effect of Lipid-Lowering Therapy on Lipoprotein and Lipid Values. Cardiovasc Drugs Ther. 2013;27(5):465-479. doi:10.1007/s10557-013-6477-6
21. Bays H, Conard S, Leiter LA, et al. Are post-treatment low-density lipoprotein subclass pattern analyses potentially misleading? Lipids Health Dis. 2010;9:136. doi:10.1186/1476-511X-9-136
22. Zhang S, Zhou Y, Wang J, et al. The Association of High Lipoprotein(a) Concentration and Risk of Ischaemic Stroke in Atrial Fibrillation Patients. Int J Gen Med. 2024;17:2001-2009. doi:10.2147/IJGM.S449400
23. Teoli J, Chikh K, Jouini-Bouhamri R, et al. When discordant insulin and C-peptide levels lead to a medical diagnosis in a patient with transient hypoglycemia: Varying degrees of interference of insulin-antibody complexes on three insulin immunoassays. Heliyon. 2024;10(13):e34009. doi:10.1016/j.heliyon.2024.e34009
24. Gao Q, Wang Q, Gan Z, et al. Fasting plasma glucose levels are associated with all-cause and cancer mortality: A population-based retrospective cohort study. PLoS One. 2024;19(11):e0311150. doi:10.1371/journal.pone.0311150
25. Gao W, Jin Y, Wang M, et al. Case Report: Abnormally Low Glycosylated Hemoglobin A1c Caused by Clinically Silent Rare β-Thalassemia in a Tujia Chinese Woman. Front Endocrinol (Lausanne). 2022;13:878680. doi:10.3389/fendo.2022.878680
26. Aydin E, Ozkokeli M. Does Homeostasis Model Assessment of Insulin Resistance have a predictive value for post-coronary artery bypass grafting surgery outcomes? Rev Bras Cir Cardiovasc. 2014;29(3):360-366. doi:10.5935/1678-9741.20140105
27. Matone A, Derlindati E, Marchetti L, et al. Identification of an early transcriptomic signature of insulin resistance and related diseases in lymphomonocytes of healthy subjects. PLoS One. 2017;12(8):e0182559. doi:10.1371/journal.pone.0182559
28. Gholami Z, Clark CCT, Paknahad Z. The effect of psyllium on fasting blood sugar, HbA1c, HOMA IR, and insulin control: a GRADE-assessed systematic review and meta-analysis of randomized controlled trials. BMC Endocr Disord. 2024;24:82. doi:10.1186/s12902-024-01608-2
29. Badaam KM, Zingade US. The Effect of Traditional Aerobic Exercise and Sprint Interval Training on Insulin Resistance in Men With Prediabetes: A Randomised Controlled Trial. Cureus. 13(12):e20789. doi:10.7759/cureus.20789
30. Cheng M, Cheng M, Wei Q. Association of myeloperoxidase, homocysteine and high-sensitivity C-reactive protein with the severity of coronary artery disease and their diagnostic and prognostic value. Exp Ther Med. 2020;20(2):1532-1540. doi:10.3892/etm.2020.8817
31. Wang Z, Tang J, Shi Q, et al. Synergistic effect of lipoprotein(a) and high-sensitivity C-reactive protein on the risk of all-cause and cardiovascular death in patients with acute myocardial infarction: a large prospective cohort study. Front Endocrinol (Lausanne). 2024;15:1392859. doi:10.3389/fendo.2024.1392859
32. Hamlin MJ, Fraser M, Lizamore CA, et al. Measurement of Cardiorespiratory Fitness in Children from Two Commonly Used Field Tests After Accounting for Body Fatness and Maturity. J Hum Kinet. 2014;40:83-92. doi:10.2478/hukin-2014-0010
33. Väisänen D, Ekblom B, Wallin P, et al. Reference values for estimated VO2max by two submaximal cycle tests: the Åstrand-test and the Ekblom-Bak test. Eur J Appl Physiol. 2024;124(6):1747-1756. doi:10.1007/s00421-023-05398-8
34. NHS Health Check. nhs.uk. November 6, 2023. Accessed June 25, 2025. https://www.nhs.uk/tests-and-treatments/nhs-health-check/




