Mothers undergo a wide array of bodily changes in the first few months following giving birth. The vast majority of changes are normal; however, they can disguise the appearance of more serious problems, creating a diagnostic blind spot. These changes can include breast changes, particularly in those breastfeeding, which can mask the presence of cancer, and fatigue, which can mask anaemia or thyroid impairment1. Undergoing a health check can help to bridge this gap in women’s health.
Key Take-Home Information
- MRI scans can be more effective than mammograms when breasts are milk-dense, and are particularly recommended for those at a high risk2.
- Blood tests, including ferritin, fasting glucose, lipid panels, and vitamin panels, can flag postpartum issues.
- The best time for a postpartum health check is between 6 weeks and 6 months after giving birth.
Why Do Mammograms Fall Short?
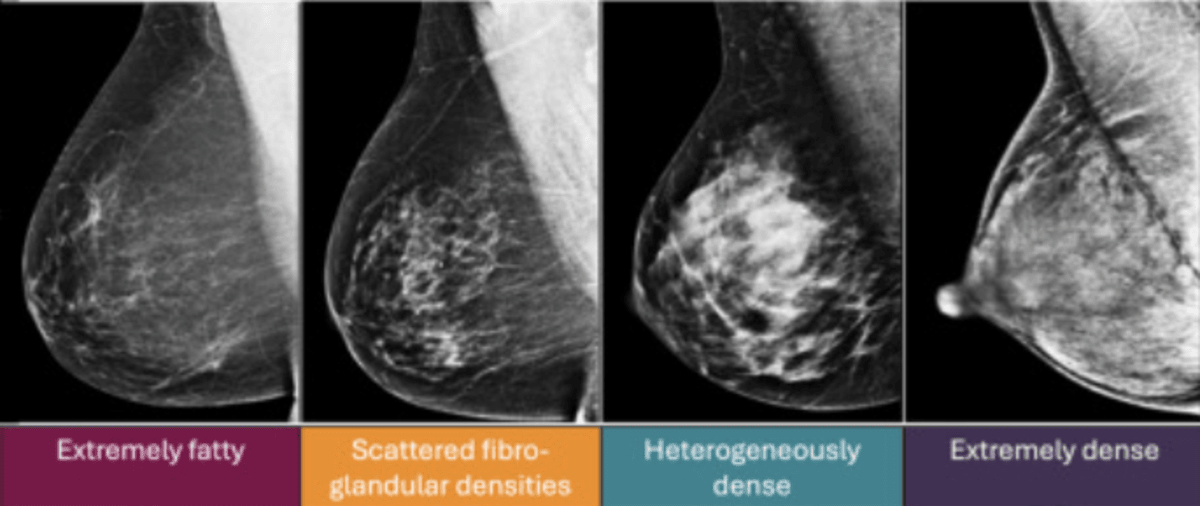
Mammograms can face issues with accuracy when imaging the breasts of postpartum women, particularly if those women are breastfeeding. During pregnancy, breasts undergo significant changes to prepare them to produce milk, including enlarged ducts and lobules (making breasts feel more lumpy) and increased breast density. The lumpiness of breastfeeding breasts can disguise the presence of new, more concerning lumps3, making women more hesitant to seek help. If they do obtain help from their doctor, their increased breast density can make mammograms more difficult and potentially less accurate4.
Postpartum Health Checks
What a Non-Contrast MRI Sees That X-Rays Miss
Mammograms use X-rays to image breast tissue and identify potentially cancerous masses. While these scans have a relatively low false positive rate (the test shows a suspicious abnormality, but after further tests is found not to be cancer) in low-density breasts, as density increases, the rate of false positives also increases5. MRI scans are sensitive to different types of soft tissue, allowing them to distinguish between dense breast tissue and potential tumours6.
Who Benefits the Most?
Breast MRIs are considered most beneficial for those who are at a high risk of developing breast cancer, including women with7:
- BRCA gene mutations
- A strong family history of breast cancer
- Dense breast tissue
In these circumstances, it is recommended that women get regular screenings from a younger age than is otherwise recommended. However, the repeated exposure to X-rays in mammograms can cause harm, and so mammograms are generally not offered to women under 357. In these situations, MRI can be used as a safe alternative with increased accuracy in dense tissue.
Safety Concerns
MRIs do not involve radiation and are therefore safe for regular screenings8. MRIs are also thought to be safe during pregnancy, with no reliable evidence demonstrating any harm to the baby9, and are breastfeeding compatible.
Cost and Access
Women in high-risk groups may be eligible for routine breast MRIs on the NHS, including those with BRCA mutations. Women not eligable for scans on the NHS may have to pay to go to a private clinic. Developments in the technology used in MRIs are resulting in the prices of MRIs decreasing, with companies like Ezra offering an MRI Scan with Spine for £2,395.
Blood Panels
Ferritin
Postpartum women are prone to iron deficiency due to reduced iron stores from pregnancy and blood loss during delivery10. To detect iron deficiency, a ferritin blood test can be carried out11.
Thyroid-Stimulating Hormone (TSH)
Thyroid problems are common in postpartum women, with symptoms such as fatigue, mood changes, and weight changes often mistaken for normal postpartum recovery12. A TSH blood test can be used to find thyroid problems13.
Fasting Glucose
Gestational diabetes (GDM; diabetes which develops whilst pregnant) is relatively common, and usually resolves soon after delivery. However, a small proportion of women who experienced GDM may have continuing problems postpartum, and all women with GDM are at an increased risk of developing Type 2 diabetes in the future14,15. Fasting glucose levels can be assessed to identify high blood sugar and potential prediabetes or diabetes16.
Lipid Panel
Pregnant women experience a rise in lipids in their blood, including LDL-cholesterol and triglycerides, to support the growth of the baby. These generally decrease rapidly after delivery, returning to pre-pregnancy levels. However, in some women, levels can remain elevated for up to a year post-delivery17,18. Persistently high levels of lipids or altered lipid ratios can increase women’s risk of developing heart disease19. Testing a lipid panel, including LDL-cholesterol, total cholesterol, and triglycerides, can provide information on women’s postpartum lipid rebound.
Vitamin and Mineral Deficiencies
Women are susceptible to vitamin and mineral deficiencies postpartum due to the demands on the body of pregnancy, blood loss during delivery, and the transfer of nutrients to the baby through breastfeeding. Deficiencies in Vitamin D and Vitamin B12 are particularly common, potentially contributing to postpartum depression, fatigue, and brain fog20–22.
Summary
Women’s bodies change significantly during pregnancy and can take time to return to a pre-pregnancy state. During this time (approximately 6 weeks to 6 months), women are in a diagnostic blind spot. A postpartum health check during this period can be beneficial. This may include an MRI to check for masked breast tumours, and blood tests to assess how women’s bodies are recovering post-pregnancy.
If you want to be proactive about your health, why not book an Ezra full-body MRI? Our annual scan catches potential cancer earlier: leveraging AI through the screening process to make it more efficient, affordable, and faster.
Understand your risk for cancer with our 5 minute quiz.
Our scan is designed to detect potential cancer early.
References
1. Yefet E, Suleiman A, Garmi G, Hatokay A, Nachum Z. Evaluation of postpartum anaemia screening to improve anaemia diagnosis and patient care: A prospective non-randomized before-and-after anaemia screening protocol implementation study. Sci Rep. 2019;9(1):7810. doi:10.1038/s41598-019-44334-9
2. Nissan N, Gluskin J, Ochoa-Albiztegui RE, Fruchtman-Brot H, Sung JS, Jochelson MS. Performance of breast MRI for high-risk screening during lactation. Eur Radiol. 2025;35(5):2366-2375. doi:10.1007/s00330-024-11091-x
3. Petok ES. Breast cancer and breastfeeding: five cases. J Hum Lact Off J Int Lact Consult Assoc. 1995;11(3):205-209. doi:10.1177/089033449501100322
4. Understanding How Pregnancy and Breastfeeding Impact Breast Imaging and Diagnosis. Accessed August 12, 2025. https://www.rsna.org/news/2023/september/pregnancy-breastfeeding-breast-imaging
5. Wanders JOP, Holland K, Veldhuis WB, et al. Volumetric breast density affects performance of digital screening mammography. Breast Cancer Res Treat. 2017;162(1):95-103. doi:10.1007/s10549-016-4090-7
6. Bakker MF, Lange SV de, Pijnappel RM, et al. Supplemental MRI Screening for Women with Extremely Dense Breast Tissue. N Engl J Med. 2019;381(22):2091-2102. doi:10.1056/NEJMoa1903986
7. Schoub PK. Understanding indications and defining guidelines for breast magnetic resonance imaging. SA J Radiol. 2018;22(2):1353. doi:10.4102/sajr.v22i2.1353
8. MRI scan. nhs.uk. October 23, 2017. Accessed August 12, 2025. https://www.nhs.uk/tests-and-treatments/mri-scan/
9. Radiology (ACR) RS of NA (RSNA) and AC of. MRI Safety During Pregnancy. Radiologyinfo.org. Accessed August 12, 2025. https://www.radiologyinfo.org/en/info/safety-mri-pregnancy
10. Neef V, Choorapoikayil S, Hof L, Meybohm P, Zacharowski K. Current concepts in postpartum anemia management. Curr Opin Anaesthesiol. 2024;37(3):234-238. doi:10.1097/ACO.0000000000001338
11. Khalafallah AA, Dennis AE. Iron Deficiency Anaemia in Pregnancy and Postpartum: Pathophysiology and Effect of Oral versus Intravenous Iron Therapy. J Pregnancy. 2012;2012:630519. doi:10.1155/2012/630519
12. Naji Rad S, Deluxe L. Postpartum Thyroiditis. In: StatPearls. StatPearls Publishing; 2025. Accessed August 12, 2025. http://www.ncbi.nlm.nih.gov/books/NBK557646/
13. Thyroid function tests. British Thyroid Foundation. September 10, 2022. Accessed August 12, 2025. https://www.btf-thyroid.org/thyroid-function-tests
14. Inoue H, Ishikawa K, Takeda K, et al. Postpartum risk of diabetes and predictive factors for glucose intolerance in East Asian women with gestational diabetes. Diabetes Res Clin Pract. 2018;140:1-8. doi:10.1016/j.diabres.2018.03.031
15. Lawrence JM, Black MH, Hsu JW, Chen W, Sacks DA. Prevalence and Timing of Postpartum Glucose Testing and Sustained Glucose Dysregulation After Gestational Diabetes Mellitus. Diabetes Care. 2010;33(3):569-576. doi:10.2337/dc09-2095
16. High blood sugar (hyperglycaemia). nhs.uk. October 18, 2017. Accessed August 12, 2025. https://www.nhs.uk/conditions/high-blood-sugar-hyperglycaemia/
17. Tan EC, Dias JM, Nicklas JM, Seely EW. 6956 Changes in LDL-Cholesterol from 6 Weeks to 12 Months Postpartum in Women with Recent Gestational Diabetes. J Endocr Soc. 2024;8(Supplement_1):bvae163.565. doi:10.1210/jendso/bvae163.565
18. Prairie BA, Wisniewski SR, Luther JF, Sit D, Wisner KL. Postpartum Lipid Levels in Women with Major Depression. J Womens Health. 2012;21(5):534-538. doi:10.1089/jwh.2011.3256
19. Markovitz AR, Haug EB, Horn J, et al. Does pregnancy alter life-course lipid trajectories? Evidence from the HUNT Study in Norway. J Lipid Res. 2018;59(12):2403-2412. doi:10.1194/jlr.P085720
20. Vitamin B12 or folate deficiency anaemia - Symptoms. nhs.uk. October 20, 2017. Accessed August 12, 2025. https://www.nhs.uk/conditions/vitamin-b12-or-folate-deficiency-anaemia/symptoms/
21. Ogiji J, Rich W. An exploratory study of vitamin D levels during pregnancy and its association with postpartum depression. Psychiatry Res Commun. 2022;2(1):100021. doi:10.1016/j.psycom.2022.100021
22. Dhiman P, Pillai RR, Wilson AB, et al. Cross-sectional association between vitamin B12 status and probable postpartum depression in Indian women. BMC Pregnancy Childbirth. 2021;21:146. doi:10.1186/s12884-021-03622-x