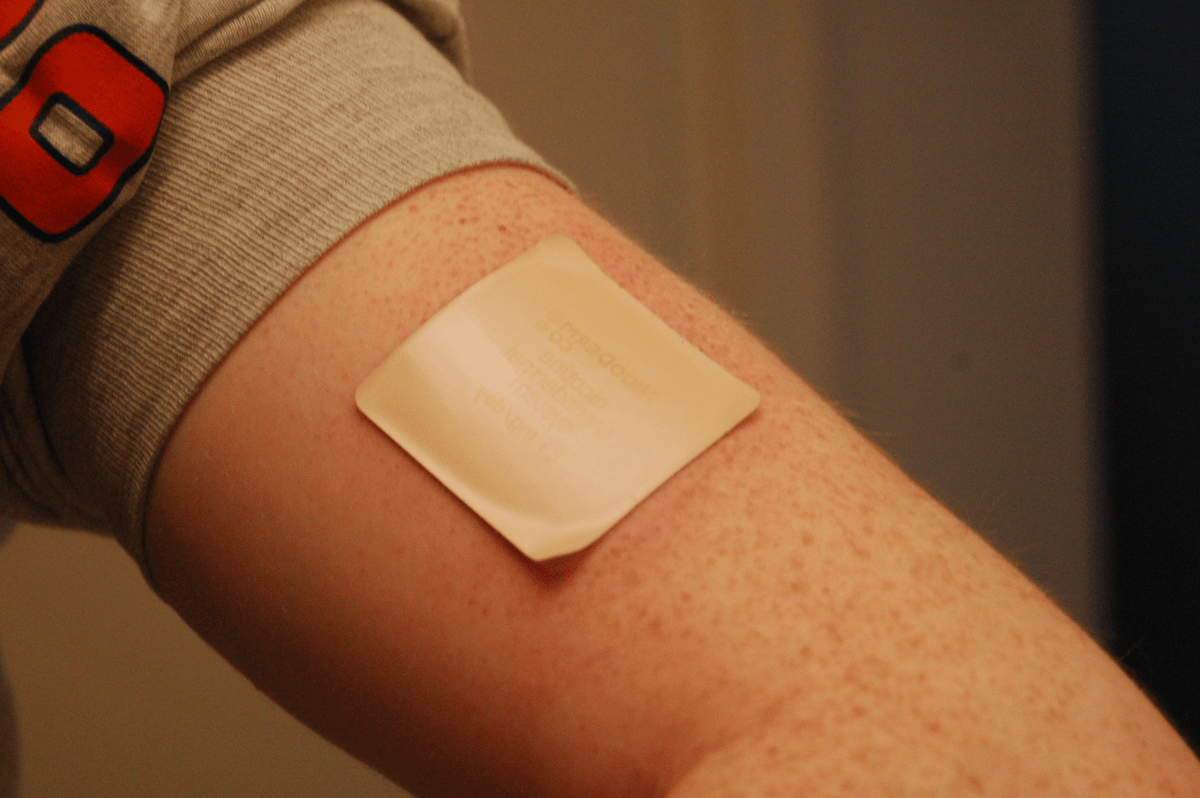
Is managing hormonal decline really as simple as wearing a patch? Emerging evidence suggests it could be. In recent years, a UK repurposing study known as the PATCH trial has investigated whether oestradiol patches could safely replace standard hormone injections in men with prostate cancer1. Meanwhile, menopause patches are being actively used as an alternative to oral hormone replacement therapy (HRT)2–4. This article explores how transdermal hormone delivery works and why steady skin-based dosing may help reduce adverse side effects in ageing adults.
Key facts about the PATCH trial
- Purpose: A UK-based trial comparing transdermal oestradiol patches with standard LHRH agonist injections for androgen suppression in men with prostate cancer1.
- Participants: Men with locally advanced, metastatic, or relapsing prostate cancer1.
- How patches work: Delivers oestradiol steadily through the skin, which suppresses testosterone production.
- Benefits: Oestradiol patches matched the effectiveness of standard injections while reducing the side effects of hot flushes and breast tenderness, improving bone density, and showing no excess cardiovascular risk1,5.
- 2025: Original PATCH trial follow-up is ongoing. The STAMPEDE platform trial is actively testing patches in combination therapies1.
Key facts about menopause patches
- Clinical evidence: Large observational studies and clinical guidance updates support transdermal HRT as an alternative to oral oestrogen for women, with similar efficacy and safety3.
- Populations: Women in perimenopause or menopause for symptom relief and long-term health support.
- How patches work: Steadily releases oestrogen (and sometimes progestogen) through the skin.
- Benefits: May have a lower risk of blood clots compared to oral HRT2,4.
- 2025: Widely licensed in the UK and available on NHS prescription6.
Why Hormone Levels Decline With Age
From testosterone to medical suppression
In prostate cancer, tumour cells can use testosterone as a growth signal, so blocking this hormone is key to treating advanced disease7. Traditionally, this is managed through injections of LHRH agonists or surgical removal of the testes. While effective, both approaches can trigger systemic side effects, including hot flushes, bone loss, metabolic changes, and cardiovascular strain8,9.
Menopausal hormone decline
Oestrogen levels produced by the ovaries decline sharply in women as they transition through perimenopause to menopause. Often, circulating estradiol falls by up to 90%, marking the end of menstrual cycles and fertility10, causing symptoms including hot flushes, bone loss, brain fog, and mood changes11. HRT replaces hormones that the body produces less of as women go through menopause, helping to manage symptoms6.
Transdermal Patches: How They Work
Steady release through skin
Transdermal patches contain hormones, working by slowly delivering the active compound across the skin into the systemic circulation through skin capillaries. This avoids first-pass metabolism in the liver, resulting in a steady and sustained release of hormones12.
Potential benefits to health
Oral HRT has been linked to an increased risk of blood clots and stroke13, while some studies report that transdermal delivery may help reduce clotting risk2,4. Early findings from prostate cancer trials show hormone patches had comparable suppression of testosterone as injectable methods, but showed fewer adverse side effects, including hot flushes and breast swelling, and may improve bone density5.
Who’s already using them?
Transdermal patches like Estradot contain oestrogen and are widely used in menopause symptom management. Some patches, like Evorel Conti, contain oestrogen as well as progestogen to protect the womb lining. For the treatment of prostate cancer, since the PATCH trial, oestradiol transdermal patches have gained attention and are being considered as treatment options for prostate cancer5. Transdermal patches are also being explored for testosterone replacement for menopausal women, however, these are not currently licensed in the UK6.
Longevity Benefits of Hormonal Balance
Brain and cognitive health
Oestrogen supports memory, processing speed, and mood regulation, so a sudden decline may increase the risk of cognitive, sleep, and mood changes14. Steady replacement may preserve neuroprotection, especially post-menopause.
Bone density & fracture risk
Both men and women experience a decline in bone density as hormone levels decrease. HRT has been shown to reduce the risk of spine, hip, and osteoporotic fractures15, while hormone patches for prostate cancer have been shown to improve bone density5.
Cardiovascular risk
Some studies suggest that oestradiol patches may be a safer alternative to oral HRT due to reduced risk of blood clots2,4. In prostate cancer patients, hormone patches have been reported to have the same cardiovascular side effects as injectable hormone methods1,5.
Should You Ask About a Patch?
- For women: Patches are recommended by NICE as HRT for many postmenopausal symptoms.
- For men: Oestradiol patch trials for prostate cancer are still underway, but early data are promising.
Always consult with a healthcare provider or hormone specialist before starting any hormonal therapy. At Ezra, our MRI scans provide structural insights into organs involved in hormonal health, including the uterus, adrenal glands, prostate, and ovaries. Getting a complete picture of your health first can help guide safer, more informed decisions about hormone treatment.
Conclusion
Transdermal patches aren’t new, but they’re finally getting the credit they deserve in hormone care. Whether you're navigating menopause or managing prostate cancer, patches may offer a steadier and safer way to balance hormones and support long-term health. As the science evolves, your skin might just be the smartest way to deliver what ageing bodies need most.
Want to explore how ageing is affecting your internal health? An Ezra MRI Scan with Spine can detect subtle structural changes in up to 14 organs, from the adrenal glands to the brain.
Understand your risk for cancer with our 5 minute quiz.
Our scan is designed to detect potential cancer early.
References
1. Gilbert DC, Nankivell M, Rush H, et al. A Repurposing Programme Evaluating Transdermal Oestradiol Patches for the Treatment of Prostate Cancer Within the PATCH and STAMPEDE Trials: Current Results and Adapting Trial Design. Clin Oncol. 2024;36(1):e11-e19. doi:10.1016/j.clon.2023.10.054
2. Laliberté F, Dea K, Duh MS, Kahler KH, Rolli M, Lefebvre P. Does the route of administration for estrogen hormone therapy impact the risk of venous thromboembolism? Estradiol transdermal system versus oral estrogen-only hormone therapy. Menopause. 2018;25(11):1297-1305. doi:10.1097/GME.0000000000001232
3. Tang R, Xie Z, Ruan X, et al. Changes in menopausal symptoms comparing oral estradiol versus transdermal estradiol. Climacteric. 2024;27(2):171-177. doi:10.1080/13697137.2023.2273530
4. Goldštajn MŠ, Mikuš M, Ferrari FA, et al. Effects of transdermal versus oral hormone replacement therapy in postmenopause: a systematic review. Arch Gynecol Obstet. 2022;307(6):1727-1745. doi:10.1007/s00404-022-06647-5
5. UKRI MRC Clinical Trials Unit UCL. Hormone patches are as effective as hormone injections for people with non-metastatic prostate cancer. September 16, 2024. Accessed August 13, 2025. https://www.mrcctu.ucl.ac.uk/news/news-stories/2024/september/hormone-patches-are-as-effective-as-hormone-injections-for-people-with-non-metastatic-prostate-cancer/#:~:text=Standard%20hormone%20therapy%20injections%20can,heart%20disease%20in%20the%20future.
6. NHS. Types of hormone replacement therapy (HRT). March 9, 2023. Accessed August 13, 2025. https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/types-of-hormone-replacement-therapy-hrt/
7. Cancer Research UK. Hormone therapy for prostate cancer. July 2, 2025. Accessed August 13, 2025. https://www.cancerresearchuk.org/about-cancer/prostate-cancer/treatment/hormone-therapy
8. Miller JI, Ahmann FR. Treatment of castration-induced menopausal symptoms with low dose diethylstilbestrol in men with advanced prostate cancer. Urology. 1992;40(6):499-502. doi:10.1016/0090-4295(92)90401-H
9. Kumar RJ, Barqawi A, Crawford ED. Adverse events associated with hormonal therapy for prostate cancer. Rev Urol. 2005;7 Suppl 5(Suppl 5):S37-43.
10. Burger HG. Physiology and endocrinology of the menopause. Medicine (Baltimore). 2006;34(1):27-30. doi:10.1383/medc.2006.34.1.27
11. Santoro N, Roeca C, Peters BA, Neal-Perry G. The Menopause Transition: Signs, Symptoms, and Management Options. J Clin Endocrinol Metab. 2021;106(1):1-15. doi:10.1210/clinem/dgaa764
12. Hupfeld S, Gravem H. Depotplastre som administrasjonsprinsipp for legemidler. Tidsskr Den Nor Legeforening. 2009;129(6):532-533. doi:10.4045/tidsskr.09.33349
13. NHS. Benefits and risks of hormone replacement therapy (HRT). February 8, 2023. Accessed August 13, 2025. https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/benefits-and-risks-of-hormone-replacement-therapy-hrt/
14. Russell JK, Jones CK, Newhouse PA. The Role of Estrogen in Brain and Cognitive Aging. Neurother J Am Soc Exp Neurother. 2019;16(3):649-665. doi:10.1007/s13311-019-00766-9
15. Stevenson J, in collaboration with the medical advisory council of the British Menopause Society. Prevention and treatment of osteoporosis in women. Post Reprod Health. 2023;29(1):11-14. doi:10.1177/20533691221139902