An MRI scan of the adrenal glands is a detailed, radiation-free imaging test used to assess small glands located above each kidney. It plays a vital role in detecting tumours and determining whether they are benign (non-cancerous) or malignant (cancerous). MRI demonstrates high sensitivity and specificity for detecting adrenal lesions and is particularly valuable for characterizing masses that cannot be definitively identified by computed tomography (CT)1,2.
An adrenal gland MRI might be recommended for several clinical reasons:
If a previous CT or ultrasound scan showed a small growth (called an incidentaloma), an MRI can assist in the confirmation of this3. MRI can also show whether it’s likely to be a harmless fatty lump (adenoma) or something that needs further follow-up.
Sometimes blood or urine tests show that the adrenal glands are making too much of certain hormones, like cortisol or adrenaline. This can cause symptoms like high blood pressure, weight changes, or anxiety. An MRI helps identify whether a small tumour is behind these changes4.
People who have or have had cancer may need an adrenal MRI to see if cancer cells have spread to these glands. Because the adrenal glands are a common place for secondary tumours to appear, this scan helps doctors plan treatment if anything new shows up. Whole-body diffusion-weighted imaging (WB-DWI), a specialised MRI technique, has shown a 100% detection rate in identifying adrenal gland metastases, confirming its high sensitivity for metastatic detection5.
MRI can also be used for the following6,7:
Here are a few tips to help you prepare for your MRI8:
You can read more about preparation for Ezra’s MRI Scan with Spine here.
Upon arrival for your abdominal MRI for the adrenal glands, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the scan, you will lie down on a sliding table. A dedicated surface or phased-array coil is typically placed over the limb or region of interest9. Your head will be nestled in a small cushion that will keep you still. The scan typically lasts 30-45 minutes of actual “table time”, during which the technician may acquire multiple sequences (settings). Expect loud knocking noises (up to 110 dB); earplugs or headphones are provided to reduce discomfort. It’s normal to feel mild table vibrations.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the coil is removed, and you’re free to go.
At Ezra, our MRI Scan with Spine scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
After the scan, you will be contacted by a medical provider working with Ezra within roughly a week. On the day of the appointment, you will receive a copy of your report and access to your scanned images through the online portal.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
MRI reports of the adrenal gland include specific terms that help clinicians assess the nature of a lesion or condition. Some common terms (and their meanings) include:
Lipid Rich: This means that the lump has a lot of fat inside its cells, which is typical for harmless (benign) adrenal adenomas16. Seeing this term suggests that the lesion is not cancerous.
Heterogeneous: If a lesion is described as heterogeneous, it means there are different types of tissues or areas within it. Mixed signals can sometimes mean the lesion is more complex and may raise suspicion for cancer, but not always; further tests or follow-up might be needed17.
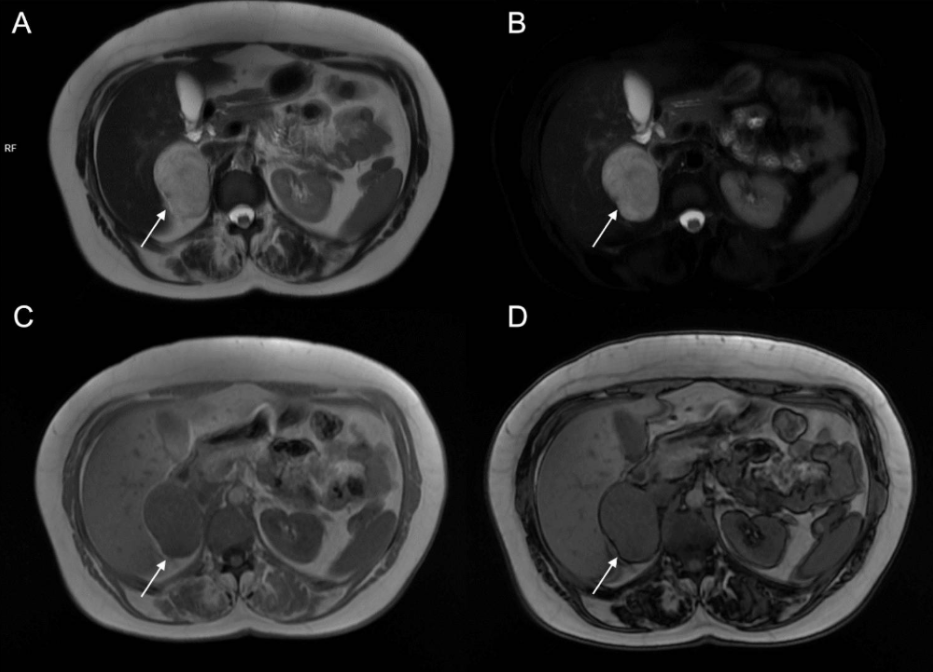
Signal Drop on Out-of-Phase Imaging: This is a technical phrase used by radiologists. It means that, when certain MRI pictures are taken (so-called “out-of-phase” images), the spot becomes less visible or darker, which is a classic sign of a fat-rich (lipid-rich) adenoma, and usually points toward a benign lump17.
Necrosis or Haemorrhage: Necrosis means part of the lesion has died due to lack of blood flow; haemorrhage means bleeding within the lump17. Either finding can be a warning sign for an aggressive or cancerous tumour, but can also occur in some benign tumours, so context matters.
Washout Pattern: This describes how quickly a contrast dye leaves the lesion during the scan. Radiologists use this to help tell the difference between types of lumps18. The washout rate can help decide whether a lesion behaves like a benign adenoma or something more concerning.
Ezra provides a radiologist-reviewed report in a non-technical and easy-to-understand format on your dashboard.
After the MRI scan, you will be free to go home and continue with your day without any precautions19. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol, or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI is a crucial tool for evaluating adrenal gland tumours, giving doctors the ability to evaluate important features like size, structure, and tissue characteristics of lesions.
This is a common, harmless lump that usually doesn’t cause symptoms. On MRI, they show a characteristic loss of signal on special out-of-phase sequences because the fat cancels out the signal from water20. This helps distinguish them from other tumours. They usually appear small, smooth, and uniform.
A benign mass that contains little or no fat, so they do not show the typical signal loss on out-of-phase MRI21. They can be harder to tell apart from malignant tumours because their MRI appearance is less specific. Their shape is usually well-defined but may vary.
An ACC is a rare and aggressive cancer of the adrenal cortex. On MRI, it tends to be a large, irregular mass with mixed signals caused by areas of bleeding or dead tissue22. It often enhances unevenly after contrast injection, unlike benign adenomas.
MRI is used to detect adrenal cancers, including adrenocortical carcinoma or secondary tumours (metastases) from cancers in other parts of the body23. Cancerous lesions typically appear larger, with irregular or heterogeneous structure, areas of necrosis, and possible haemorrhage.
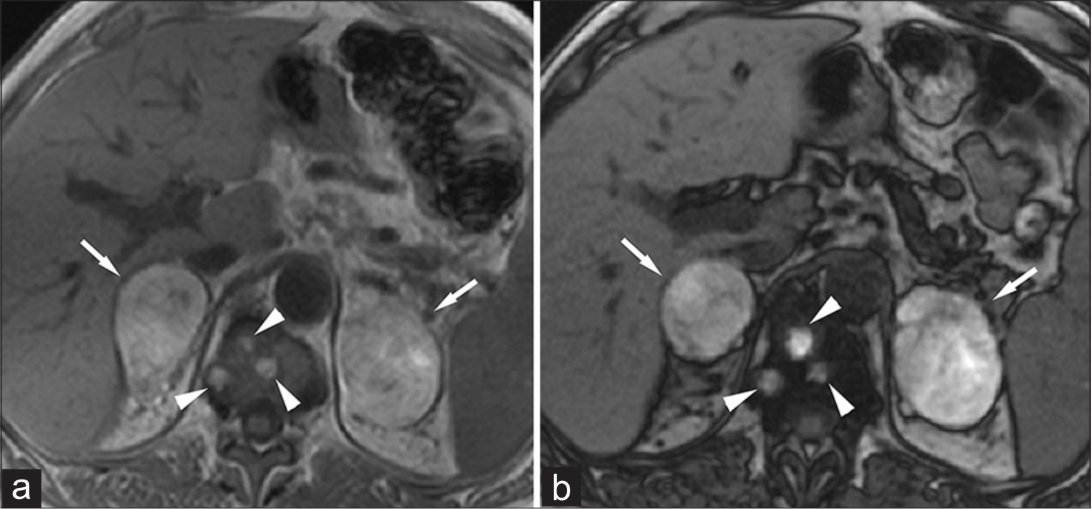
Phaeochromocytomas are tumours originating from the adrenal medulla and often produce excess adrenaline. They are classically bright on T2-weighted MRI images, the so-called “light bulb” sign, and enhance strongly after contrast24.
Myelolipomas are benign lesions made of fat and bone marrow cells, showing high signal intensity on T1-weighted MRI sequences because of their fat content. They lose signal on fat-suppressed images, making them easily identifiable compared to other adrenal masses26.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London, and in Sidcup, with more locations planned in the future. No referral is required, so you can book your scan directly without consulting a GP or specialist first. Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
Yes, adrenal MRI is generally safe for most people and does not use harmful radiation, though people with certain metal implants or severe claustrophobia should discuss risks with their doctor.
Contrast dye is often recommended to improve tumour visibility, but it may not be needed in all cases and depends on your doctor’s assessment.
Yes, if no sedatives were given; if you received sedatives for anxiety or discomfort, you should not drive and need someone to assist you home.
No, the images are reviewed by a radiologist after the scan, so results typically take a few days, and your doctor will explain them to you.



1. Hrabak-Paar M, Đido V, Štern-Padovan R. Should we use CT or MRI for detection and characterization of benign adrenal lesions? Ann Endocrinol (Paris). 2015;76(3):272-280. doi:10.1016/j.ando.2015.03.040
2. Derlin T, Busch JD, Wisotzki C, et al. Intraindividual comparison of 123I-mIBG SPECT/MRI, 123I-mIBG SPECT/CT, and MRI for the detection of adrenal pheochromocytoma in patients with elevated urine or plasma catecholamines. Clin Nucl Med. 2013;38(1):e1-6. doi:10.1097/RLU.0b013e318263923d
3. Owei L, Wachtel H. The Landmark Series: Evaluation and Management of Adrenal Incidentalomas. Ann Surg Oncol. 2025;32(7):4712-4719. doi:10.1245/s10434-025-17296-8
4. Hayashi M, Kataoka Y, Sugimura Y, et al. A 68-year-old phenotypically male patient with 21-hydroxylase deficiency and concomitant adrenocortical neoplasm producing testosterone and cortisol. Tohoku J Exp Med. 2013;231(2):75-84. doi:10.1620/tjem.231.75
5. Akdal Dolek B, Sozmen Ciliz D, Ozdemir N, Ozet G, Duran S. Comparative Analysis of Whole-Body Diffusion-Weighted Imaging and PET/CT in Metastasis Detection: A Prospective Study. Cureus. 16(11):e74756. doi:10.7759/cureus.74756
6. Manganaro L, Al Ansari N, Barchetti F, et al. Bilateral Adrenal Hemorrhage in a Patient with Myelodysplastic Syndrome: Value of MRI in the Differential Diagnosis. Case Rep Radiol. 2013;2013:479836. doi:10.1155/2013/479836
7. Huang YC, Tang YL, Zhang XM, Zeng NL, Li R, Chen TW. Evaluation of primary adrenal insufficiency secondary to tuberculous adrenalitis with computed tomography and magnetic resonance imaging: Current status. World J Radiol. 2015;7(10):336-342. doi:10.4329/wjr.v7.i10.336
8. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
9. Gruber B, Froeling M, Leiner T, Klomp DWJ. RF coils: A practical guide for nonphysicists. J Magn Reson Imaging. 2018;48(3):590-604. doi:10.1002/jmri.26187
10. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
11. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
12. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
13. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
14. Gamberini MR, Prandini N, Chiodi E, Farneti C, Garani MC. Adrenal incidentaloma in thalassemia: a case report and literature review. Pediatr Endocrinol Rev. 2011;8 Suppl 2:324-330.
15. Mall MA, Stahl M, Graeber SY, Sommerburg O, Kauczor HU, Wielpütz MO. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
16. Hao M, Luque-Fernandez MA, Lopez D, et al. Benign Adrenocortical Tumors and the Detection of Nonadrenal Neoplasia. Int J Endocrinol. 2019;2019:9035407. doi:10.1155/2019/9035407
17. Bracci B, De Santis D, Del Gaudio A, et al. Adrenal Lesions: A Review of Imaging. Diagnostics (Basel). 2022;12(9):2171. doi:10.3390/diagnostics12092171