A bladder magnetic resonance imaging (MRI) scan is a safe, noninvasive imaging technique providing high-resolution images of the bladder and surrounding tissues, making it particularly valuable for the detection and staging of bladder cancer. Compared to traditional methods like computed tomography (CT) or cytoscopy, MRI offers superior soft-tissue contrast and can more accurately assess whether the cancer has invaded the bladder’s muscular layer, an essential factor for determining treatment options1.
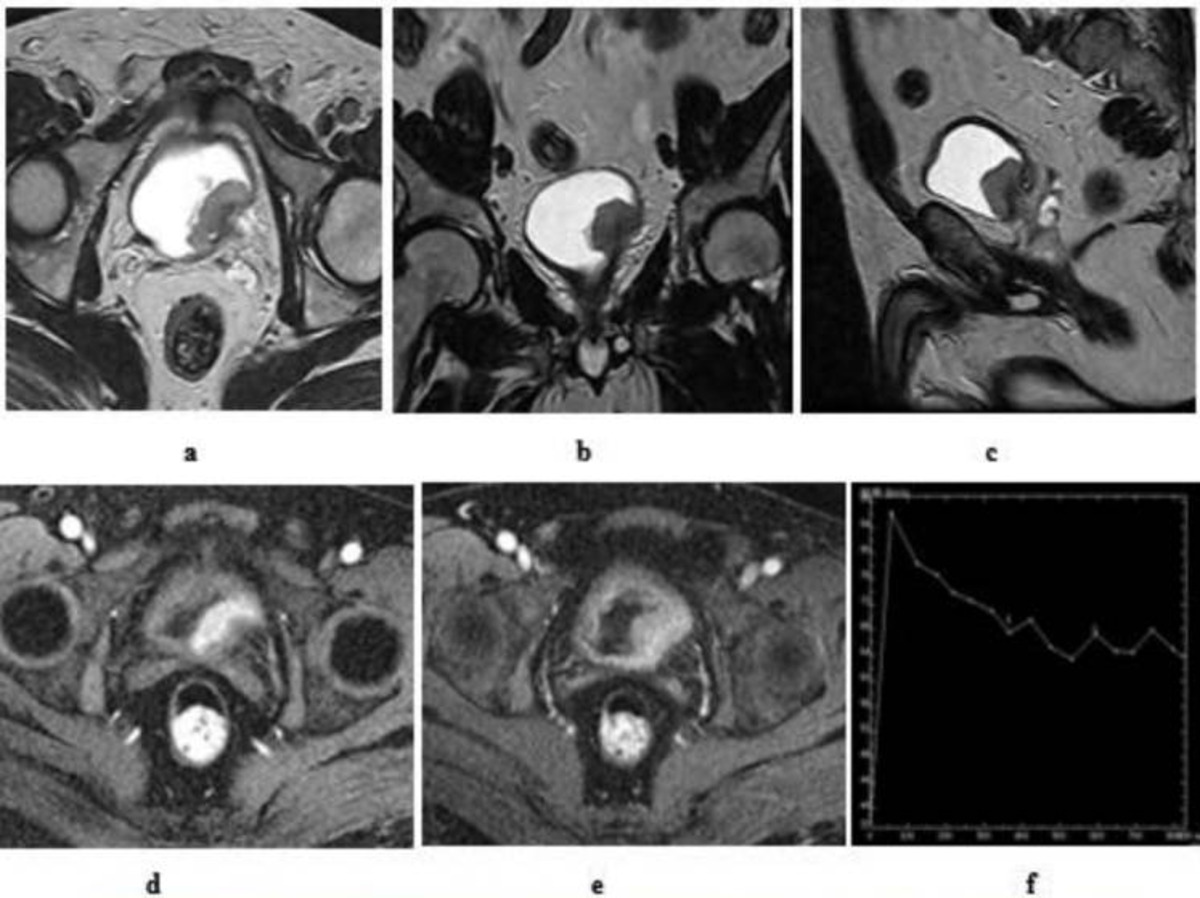
Multiparametric MRI (mpMRI), which incorporates functional sequences like diffusion-weighted imaging (DWI) and dynamic contrast-enhanced imaging, is especially effective for staging and evaluating response to treatment2. Bladder MRI is safe, uses no ionising radiation, and may also identify subtle abnormalities or infiltrative disease missed by other modalities.
A bladder MRI might be recommended for several reasons:
Here are a few tips to help you prepare for your MRI8:
You can read more about preparation for Ezra’s MRI Scan with Spine here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the scan, you will lie down on a sliding table. A dedicated surface or phased-array coil is typically placed over the limb or region of interest9. Your head will be nestled in a small cushion that will keep you still. The scan typically lasts 30-45 minutes of actual “table time”, during which the technician may acquire multiple sequences (settings). Expect loud knocking noises (up to 110 dB); earplugs or headphones are provided to reduce discomfort. It’s normal to feel mild table vibrations.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the coil is removed, and you’re free to go.
At Ezra, our MRI Scan with Spine scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
After the scan, you will be contacted by a medical provider working with Ezra within roughly a week. On the day of the appointment, you will receive a copy of your report and access to your scanned images through the online portal.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
MRI reports of the bladder include specific terms that help clinicians assess the nature of a lesion or condition. Some common terms (and their meaning) include:
VI-RADS Score: This stands for Vesical Imaging-Reporting and Data System, a standardised scale from 1 to 5 that assesses the likelihood a bladder tumour has invaded the muscle layer16. A score of 1 is very unlikely, while 5 is highly likely for muscle invasion.
Restricted Diffusion: This describes areas on DWI where water molecule movement is limited, often indicating dense tumour tissue. Restricted diffusion in a bladder lesion suggests higher cellularity and malignancy risk17.
ADC Value: The apparent diffusion coefficient (ADC) is a numerical value derived from DWI. Lower ADC values generally correspond to more aggressive, cellular tumours and are supportive of malignancy18.
Disruption of the Muscularis Propria: This finding suggests that the tumour has penetrated or disrupted the muscle layer of the bladder wall. It is a critical sign indicating muscle-invasive disease19.
Enhancement: Describes how much contrast (gadolinium dye) the tissue absorbs on MRI17. Early or intense enhancement is often associated with malignant or aggressive tumours, helping differentiate from benign lesions.
Multifocal Lesions: Indicates that more than one tumour is present within the bladder. Multifocality can influence staging, treatment, and prognosis20.
After the MRI scan, you will be free to go home and continue with your day without any precautions21. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol, or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI can provide comprehensive information about bladder cancer, aiding diagnosis, staging, and treatment monitoring.
MRI accurately details the size, shape, and exact position of a tumour within the bladder. This assists in surgical treatment and planning. Advanced mRI techniques achieve sensitivities up to 92.3 per cent and specificities up to 94 per cent for bladder tumour detection22,23.
One of MRI’s greatest strengths is evaluating whether cancer has spread into the bladder’s muscle layer. The VI-RADS scoring system offers high reliability for muscle invasion, which is important for determining the best treatment path. T2-weighted imaging and DWI demonstrate sensitivity up to 100 per cent and specificity up to 91.7 per cent for detecting muscle invasion24,25.
MRI identifies whether multiple tumours (multifocal disease) are present in the bladder, which may affect management decisions. MRI demonstrates a sensitivity of 83 -100% for detecting multifocal bladder abnormalities, which are frequently associated with tumour recurrence26.
On follow-up MRIs, radiologists can assess changes in tumour size, characteristics, and signs of response to treatment, such as shrinking or less enhancement.
MRI reveals characteristic appearances for different types of bladder tumours, allowing radiologists to distinguish between tumour types and assess the extent of disease.
These tumours are confined to the innermost lining (urothelium and lamina propria) of the bladder27. These tumours often have a papillary shape, appearing as frond-like, exophytic masses projecting into the bladder cavity. The muscular layer remains intact, with no disruption seen on MRI.
MIBC can often present with a bladder wall that is thickened in one area or even throughout, instead of looking smooth and thin28. It is sometimes described as having a “leather bottle” or stiff appearance, a term called “linitis plastica-like”, because the whole wall can stiffen up. MIBC usually shows brighter on T2-weighted scans and darker on T1-weighted scans. The edges of the tumours are often not clearly defined.
This rarer, more aggressive type frequently arises in the context of chronic irritation or inflammation. MRI often shows irregular orders and may reveal areas of central necrosis (non-enhancing tissue from tumour death). It can also appear as larger infiltrative masses29.
Adenocarcinoma of the bladder is less common and tends to be located near the bladder dome. On MRI, it appears as a well-circumscribed mass with possible mucinous content or cystic areas30. It can mimic urachal remnants (leftover tissue from a tube that connects the bladder to the belly button) due to its location.
Ezra screens for over 500 conditions, including the brain.
Several specialised MRI scan types are routinely used in bladder cancer detection, each providing unique information to help diagnose, stage, and plan treatment for bladder tumours:
This sequence highlights the different layers of the bladder wall, making it easier to see how deep a tumour has grown. Tumours usually appear brighter than normal muscle, and this type of scan is important for assessing whether the muscle layer is still intact or disrupted by cancer31,32.
DWI assesses how water molecules move within tissues. Tumours tend to restrict water movement, so they stand out as areas of restricted diffusion31–33. This helps in identifying and confirming suspicious lesions, even when they are small or subtle.
This is a map derived from DWI that provides a numerical value to help separate aggressive cancers (which have lower ADC values) from less aggressive tumours. Lower ADC suggests increased tumour cell density31,32.
DCE captures images over time after a contrast dye is injected. Malignant tumours often soak up the dye earlier than normal bladder wall tissue, a sign of abnormal blood vessels31,32,34. This helps distinguish cancer from benign tissue and is useful for staging and treatment monitoring.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London, and in Sidcup, with more locations planned in the future. No referral is required, so you can book your scan directly without consulting a GP or specialist first. Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
No, it’s non-invasive and painless, though you need to stay still for the best results.
Not fully. MRI can show tumour depth and spread, but cystoscopy is still needed for biopsy and direct visualisation.
Yes, in most cases. Gadolinium contrast is widely used, but inform your care team if you have kidney disease or previous reactions.
It should take around 7-10 days from your final scan date for your results to come in. You will receive an email when your report is ready.



1. Salmanoglu E, Halpern E, Trabulsi EJ, Kim S, Thakur ML. A glance at imaging bladder cancer. Clin Transl Imaging. 2018;6(4):257-269. doi:10.1007/s40336-018-0284-9
2. Pecoraro M, Cipollari S, Messina E, et al. Multiparametric MRI for Bladder Cancer: A Practical Approach to the Clinical Application of VI-RADS. Radiology. 2025;314(3):e233459. doi:10.1148/radiol.233459
3. Wong VK, Ganeshan D, Jensen CT, Devine CE. Imaging and Management of Bladder Cancer. Cancers (Basel). 2021;13(6):1396. doi:10.3390/cancers13061396
4. Galgano SJ, Porter KK, Burgan C, Rais-Bahrami S. The Role of Imaging in Bladder Cancer Diagnosis and Staging. Diagnostics (Basel). 2020;10(9):703. doi:10.3390/diagnostics10090703
5. Rabie E, Faeghi F, Izadpanahi MH, Dayani MA. Role of Dynamic Contrast-Enhanced Magnetic Resonance Imaging in Staging of Bladder Cancer. J Clin Diagn Res. 2016;10(4):TC01-TC05. doi:10.7860/JCDR/2016/17596.7690
6. He K, Meng X, Wang Y, et al. Progress of Multiparameter Magnetic Resonance Imaging in Bladder Cancer: A Comprehensive Literature Review. Diagnostics (Basel). 2024;14(4):442. doi:10.3390/diagnostics14040442
7. Dewulf K, Richter K, Illy M, et al. Can Bladder MRI Improve the Follow-Up of Non–Muscle-Invasive Bladder Cancer by Detecting Endoscopic Invisible Recurrence? Clinical Genitourinary Cancer. 2024;22(5). doi:10.1016/j.clgc.2024.102136
8. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
9. Gruber B, Froeling M, Leiner T, Klomp DWJ. RF coils: A practical guide for nonphysicists. J Magn Reson Imaging. 2018;48(3):590-604. doi:10.1002/jmri.26187
10. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
11. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
12. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
13. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
14. Rayn KN, Hale GR, Bloom JB, et al. Incidental bladder cancers found on multiparametric MRI of the prostate gland: a single center experience. Diagn Interv Radiol. 2018;24(5):316-320. doi:10.5152/dir.2018.18102
15. Mall MA, Stahl M, Graeber SY, Sommerburg O, Kauczor HU, Wielpütz MO. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
16. Lai AL, Law YM. VI-RADS in bladder cancer: Overview, pearls and pitfalls. European Journal of Radiology. 2023;160:110666. doi:10.1016/j.ejrad.2022.110666
17. Abouelkheir RT, Abdelhamid A, Abou El-Ghar M, El-Diasty T. Imaging of Bladder Cancer: Standard Applications and Future Trends. Medicina (Kaunas). 2021;57(3):220. doi:10.3390/medicina57030220
18. Esen M, Onur MR, Akpolat N, Orhan I, Kocakoc E. Utility of ADC measurement on diffusion-weighted MRI in differentiation of prostate cancer, normal prostate and prostatitis. Quant Imaging Med Surg. 2013;3(4):210-216. doi:10.3978/j.issn.2223-4292.2013.08.06
19. Angkathunyakul N, Treepongkaruna S, Molagool S, Ruangwattanapaisarn N. Abnormal layering of muscularis propria as a cause of chronic intestinal pseudo-obstruction: A case report and literature review. World J Gastroenterol. 2015;21(22):7059-7064. doi:10.3748/wjg.v21.i22.7059
20. Simon R, Eltze E, Schäfer KL, et al. Cytogenetic analysis of multifocal bladder cancer supports a monoclonal origin and intraepithelial spread of tumor cells. Cancer Res. 2001;61(1):355-362.
21. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
22. Beer A, Saar B, Zantl N, et al. MR cystography for bladder tumor detection. Eur Radiol. 2004;14(12):2311-2319. doi:10.1007/s00330-004-2451-9
23. Bernhardt TM, Schmidl H, Philipp C, Allhoff EP, Rapp-Bernhardt U. Diagnostic potential of virtual cystoscopy of the bladder: MRI vs CT. Preliminary report. Eur Radiol. 2003;13(2):305-312. doi:10.1007/s00330-002-1444-9
24. Rosenkrantz AB, Mussi TC, Melamed J, Taneja SS, Huang WC. Bladder cancer: utility of MRI in detection of occult muscle-invasive disease. Acta Radiol. 2012;53(6):695-699. doi:10.1258/ar.2012.120069
25. Akcay A, Yagci AB, Celen S, Ozlulerden Y, Turk NS, Ufuk F. VI-RADS score and tumor contact length in MRI: A potential method for the detection of muscle invasion in bladder cancer. Clin Imaging. 2021;77:25-36. doi:10.1016/j.clinimag.2021.02.026
26. Rosenkrantz AB, Ego-Osuala IO, Khalef V, Deng FM, Taneja SS, Huang WC. Investigation of Multisequence Magnetic Resonance Imaging for Detection of Recurrent Tumor After Transurethral Resection for Bladder Cancer. Journal of Computer Assisted Tomography. 2016;40(2):201-205. doi:10.1097/RCT.0000000000000363
27. Akintelure D, Akintelure S, Al-Ibraheem HA. Emerging Role of Multiparametric MRI in the Staging of Bladder Cancer: Insights From the BladderPath Trial. Cureus. 17(7):e88623. doi:10.7759/cureus.88623
28. Han YE, Sung DJ, Cho HY, et al. Multiparametric MRI Features of Plasmacytoid Urothelial Carcinoma of the Urinary Bladder. Korean J Radiol. 2025;26(9):832-840. doi:10.3348/kjr.2025.0419
29. Park JH, Kim M, Yoon J, et al. Tumor necrosis in magnetic resonance imaging predicts urothelial carcinoma with squamous differentiation in muscle-invasive bladder carcinoma. Abdom Radiol. 2024;49(12):4341-4351. doi:10.1007/s00261-024-04317-5
30. Abouelkheir RT, Abdelhamid A, Abou El-Ghar M, El-Diasty T. Imaging of Bladder Cancer: Standard Applications and Future Trends. Medicina (Kaunas). 2021;57(3):220. doi:10.3390/medicina57030220
31. Shalaby EA, Mohamed AR, Elkammash TH, Abouelkheir RT, Housseini AM. Role of multiparametric magnetic resonance imaging in the diagnosis and staging of urinary bladder cancer. Curr Urol. 2022;16(3):127-135. doi:10.1097/CU9.0000000000000128
32. Akin O, Lema-Dopico A, Paudyal R, et al. Multiparametric MRI in Era of Artificial Intelligence for Bladder Cancer Therapies. Cancers (Basel). 2023;15(22):5468. doi:10.3390/cancers15225468
33. Carando R, Afferi L, Marra G, et al. The effectiveness of multiparametric magnetic resonance imaging in bladder cancer (Vesical Imaging-Reporting and Data System): A systematic review. Arab J Urol. 18(2):67-71. doi:10.1080/2090598X.2020.1733818
34. He K, Meng X, Wang Y, et al. Progress of Multiparameter Magnetic Resonance Imaging in Bladder Cancer: A Comprehensive Literature Review. Diagnostics. 2024;14(4):442. doi:10.3390/diagnostics14040442