Magnetic Resonance Imaging (MRI) is a non-invasive, radiation-free imaging technique that uses powerful magnets, such as those in a 3-Tesla scanner, to generate detailed images of the brain’s structure and blood vessels. MRI plays a crucial role in the early detection of brain tumours, including glioblastoma, meningioma, and brain metastasis, which collectively account for a substantial portion of primary and secondary brain cancers.
Early identification is critical: brain tumours affect over 300,000 people worldwide annually, and early-stage detection significantly improves treatment outcomes and survival rates1. Compared to other imaging methods, MRI offers superior sensitivity for identifying even small or subtle lesions, enabling clinicians to detect changes before symptoms arise2. This makes MRI an essential tool in the timely detection and management of brain abnormalities.
Learn more about MRI for cancer detection here.
You may need a brain (head) MRI for several key reasons, especially when early detection can change outcomes:
You can use our Know Your Risk Calculator to understand your risk of cancer in just five minutes.
Here are a few tips to help you prepare for your MRI10:
You can read more about preparation for Ezra’s Full Body Scan here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the scan, you will lie down on a sliding table. A lightweight head coil will act like a helmet for clear 3-Tesla images. Your head will be nestled in a small cushion that will keep you still. The scan typically lasts 30-45 minutes of actual “table time”, during which the technician may acquire multiple sequences (settings) (T1, T2, FLAIR, DWI, SWI, and sometimes perfusion or spectroscopy)11. Expect loud knocking noises (up to 110 dB); earplugs or headphones are provided to reduce discomfort. It’s normal to feel mild table vibrations.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the head coil is removed, and you’re free to go.
At Ezra our Full Body Plus scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
After the scan, you will be contacted by a medical provider working with Ezra within roughly a week. On the day of the appointment, you will receive a copy of your report and access to your scanned images through the online portal.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
There are a number of terms you might see in your MRI report after your brain scan. Here are some explanations for some common ones:
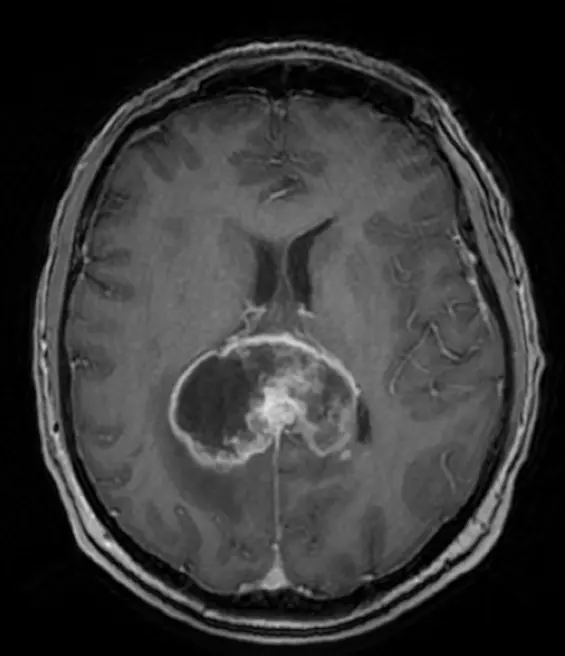
Ring-enhancing lesion: A ring-enhancing lesion appears as a bright rim surrounding a darker centre after contrast dye is administered during an MRI or CT scan18. The ring is due to contrast uptake at the edge of the lesion, often raising concern for aggressive or infectious processes.
Diffusion restriction: This term refers to areas where the movement of water molecules is blocked or restricted, as detected by DWI or MRI19. Diffusion restriction is typical of tissues with high cellularity, such as lymphoma.
rCBV (relative cerebral blood volume): rCBV is a perfusion MRI measurement indicating the amount of blood volume in a given region of brain tissue. High rCBV values suggest increased blood supply, which is often seen in high-grade tumours due to the formation of new blood vessels20.
FLAIR hyperintensity: FLAIR (Fluid-Attenuated Inversion Recovery) is an MRI sequence that highlights abnormal fluid in the brain21. It is commonly used to detect regions of abnormality, such as those caused by tumours, stroke, or inflammation.
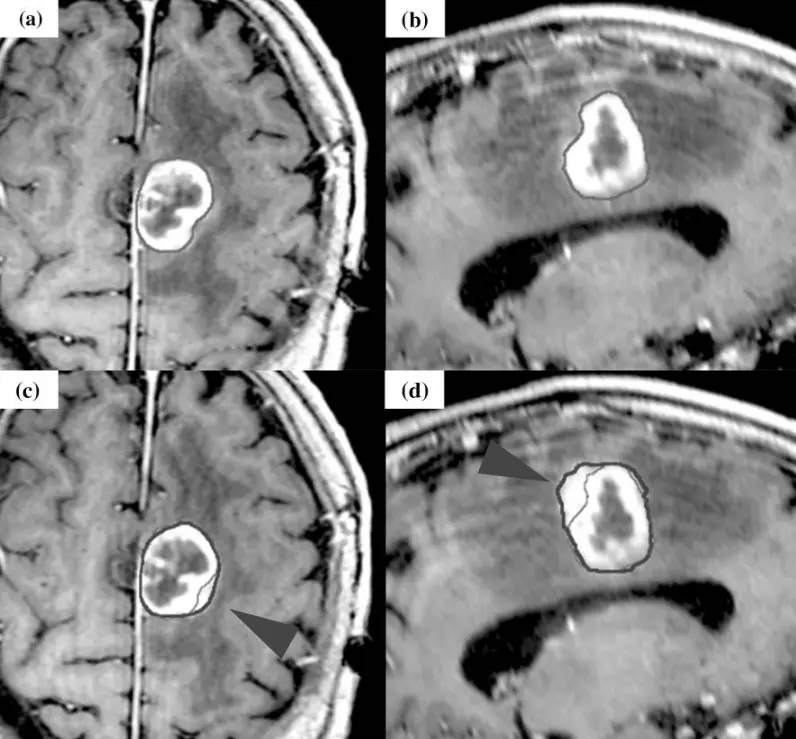
Dural tail: This is a tapered enhancement on the brain lining, which is typical of meningioma, seen in 60-72 per cent of cases22.
Calcifications: Calcifications are deposits of calcium within the brain tissue, which can be detected on MRI23. These are common in tumours like oligodendrogliomas.
Butterfly lesion: A butterfly lesion refers to a mass that crosses the midline of the brain through the corpus callosum, giving it a butterfly appearance on imaging24. This is common in glioblastomas.
Cho/NAA ratio: This is a chemical ratio measured by MR spectroscopy, comparing choline to N-acetylaspartate (a marker of healthy neurons)25. A Cho/NAA ratio >2-3 is suggestive of malignancy, as tumours tend to have increased choline and decreased NAA.
Ezra provides a radiologist-reviewed report in a non-technical and easy-to-understand format on your dashboard.
After the MRI scan, you will be free to go home and continue with your day without any precautions26. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI offers a detailed and comprehensive view of brain cancer, providing essential information for diagnosis and treatment planning. One of the key strengths of MRI is its ability to precisely pinpoint the location of a tumour, whether it’s in a specific lobe, deep brain nucleus, brainstem, or the meninges (the brain’s lining)27. This level of detail enables clinicians to identify the exact structures involved and plan the most effective intervention approach.
Different MRI sequences reveal the tumour’s internal makeup:
Certain imaging types can also show how active a tumour is. DWI assesses the movement of water molecules within brain tissue32. Tumours with restricted diffusion, appearing bright on DWI, are typically highly cellular, such as lymphomas or high-grade gliomas33. DWI is valuable for distinguishing between tumour types and grades, as well as for monitoring response to therapy34. Perfusion MRI, which measures blood flow within the tumour, provides additional information: a high rCBV is often seen in fast-growing, aggressive tumours35.
MRI is also essential for assessing the impact of a tumour on nearby brain structures. It effectively maps oedema, which appears as a high signal on T2/FLAIR images and low on T136. The presence of oedema can worsen symptoms and may be a sign of tumour aggressiveness. Additionally, MRI can identify blocked cerebrospinal fluid (CSF) pathways, which can lead to hydrocephalus, a potentially life-threatening complication37.
Ezra utilises DWI as part of our whole-body MRI scans and artificial intelligence (AI) to enhance MRI images and convert radiology reports into layman's term translations.
Ezra screens for over 500 conditions, including the brain.
There are multiple types of MRI scans, all using different methods to give a better visualisation of the brain.
The cost of a brain MRI scan on average ranges from £249 to £184553. At Ezra, we offer a full-body MRI scan that covers up to 13 organs, including the brain.
At Ezra, MRI Scan (which includes the head, neck, abdomen, and pelvis) is offered at a £1495 all-inclusive price, including a 45-minute follow-up review of your scan findings with a medical practitioner. We have a location in London, with further locations across the UK coming soon.
A standard brain MRI may include the upper part of the neck (upper cervical spine), but a full neck scan requires a dedicated cervical spine MRI.
MRI provides greater detail and sensitivity for brain abnormalities, while CT is faster and better for emergencies or bone detail; the choice depends on the clinical situation.
MRI images are available immediately after the scan, but an official radiologist's report typically takes 1-2 weeks, unless it is an emergency.
MRI cannot directly diagnose dementia, but it can reveal brain changes associated with different types of dementia, aiding in diagnosis.
You can drive home after a brain MRI unless you have received sedation, in which case you should not drive.
Consider booking an Ezra Full Body MRI Scan, which screens for up to 13 types of cancer, offering peace of mind through early detection.



1. Samman RR, Timraz JH, Mosalem Al-Nakhli A, et al. The Impact of Brain Tumors on Emotional and Behavioral Functioning. Cureus. 16(12):e75315. doi:10.7759/cureus.75315
2. Knipp SC, Matatko N, Schlamann M, et al. Small ischemic brain lesions after cardiac valve replacement detected by diffusion-weighted magnetic resonance imaging: relation to neurocognitive function. Eur J Cardiothorac Surg. 2005;28(1):88-96. doi:10.1016/j.ejcts.2005.02.043
3. Brain tumours. nhs.uk. October 17, 2017. Accessed July 1, 2025. https://www.nhs.uk/conditions/brain-tumours/
4. Irimia A, Maher AS, Rostowsky KA, et al. Brain Segmentation From Computed Tomography of Healthy Aging and Geriatric Concussion at Variable Spatial Resolutions. Front Neuroinform. 2019;13:9. doi:10.3389/fninf.2019.00009
5. Neugut AI, Sackstein P, Hillyer GC, et al. Magnetic Resonance Imaging‐Based Screening for Asymptomatic Brain Tumors: A Review. Oncologist. 2019;24(3):375-384. doi:10.1634/theoncologist.2018-0177
6. Beutler BD, Nguyen ET, Parker RA, et al. Metastatic meningioma: Case report of a WHO grade I meningioma with liver metastases and review of the literature. Radiology Case Reports. 2019;15(2):110. doi:10.1016/j.radcr.2019.10.027
7. Kleibeuker EA, Fokas E, Allen PD, et al. Low dose angiostatic treatment counteracts radiotherapy-induced tumor perfusion and enhances the anti-tumor effect. Oncotarget. 2016;7(47):76613. doi:10.18632/oncotarget.12814
8. Leone A, Carbone F, Spetzger U, et al. Preoperative mapping techniques for brain tumor surgery: a systematic review. Frontiers in Oncology. 2025;14:1481430. doi:10.3389/fonc.2024.1481430
9. Casey SO, Sampaio RC, Michel E, et al. Posterior reversible encephalopathy syndrome: utility of fluid-attenuated inversion recovery MR imaging in the detection of cortical and subcortical lesions. AJNR Am J Neuroradiol. 2000;21(7):1199-1206.
10. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
11. Brain MRI: What It Is, Purpose, Procedure & Results. Cleveland Clinic. Accessed July 1, 2025. https://my.clevelandclinic.org/health/diagnostics/22966-brain-mri
12. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
13. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
14. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
15. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
16. Rowley PA, Paukner MJ, Eisenmenger LB, et al. Incidental Findings from 16,400 Brain MRI Examinations of Research Volunteers. American Journal of Neuroradiology. 2023;44(4). Accessed July 1, 2025. https://www.ajnr.org/content/early/2023/03/16/ajnr.A7821
17. Mall MA, Stahl M, Graeber SY, et al. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
18. Tran D, Rahman Q, Weed M, et al. Differential diagnosis of a ring-enhancing brain lesion in the setting of metastatic cancer and a mycotic aneurysm. Radiol Case Rep. 2021;16(12):3850-3854. doi:10.1016/j.radcr.2021.09.041
19. Dmytriw AA, Sawlani V, Shankar J. Diffusion-Weighted Imaging of the Brain: Beyond Stroke. Canadian Association of Radiologists Journal. 2017;68(2):131-146. doi:10.1016/j.carj.2016.10.001
20. Rohilla S, Garg HK, Singh I, et al. rCBV- and ADC-based Grading of Meningiomas With Glimpse Into Emerging Molecular Diagnostics. Basic Clin Neurosci. 2018;9(6):417-428. doi:10.32598/bcn.9.6.417
21. Iancu-Gontard D, Oppenheim C, Touzé E, et al. Evaluation of Hyperintense Vessels on FLAIR MRI for the Diagnosis of Multiple Intracerebral Arterial Stenoses. Stroke. 2003;34(8):1886-1891. doi:10.1161/01.STR.0000080382.61984.FE
22. Doddamani RS, Meena RK, Sawarkar D. Ambiguity in the Dural Tail Sign on MRI. Surg Neurol Int. 2018;9:62. doi:10.4103/sni.sni_328_17
23. Wu Z, Mittal S, Kish K, et al. Identification of Calcification with Magnetic Resonance Imaging Using Susceptibility-Weighted Imaging: A Case Study. J Magn Reson Imaging. 2009;29(1):177-182. doi:10.1002/jmri.21617
24. Finneran M, Marotta DA, Altenburger D, et al. Long-term Survival in a Patient with Butterfly Glioblastoma: A Case Report. Cureus. 12(2):e6914. doi:10.7759/cureus.6914
25. Guo J, Yao C, Chen H, et al. The relationship between Cho/NAA and glioma metabolism: implementation for margin delineation of cerebral gliomas. Acta Neurochir (Wien). 2012;154(8):1361-1370. doi:10.1007/s00701-012-1418-x
26. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
27. Iijima K, Hirato M, Miyagishima T, et al. Microrecording and image-guided stereotactic biopsy of deep-seated brain tumors. J Neurosurg. 2015;123(4):978-988. doi:10.3171/2014.10.JNS14963
28. Zimny A, Zińska L, Bladowska J, et al. Intracranial lesions with high signal intensity on T1-weighted MR images – review of pathologies. Pol J Radiol. 2013;78(4):36-46. doi:10.12659/PJR.889663
29. Villanueva-Meyer JE, Mabray MC, Cha S. Current Clinical Brain Tumor Imaging. Neurosurgery. 2017;81(3):397-415. doi:10.1093/neuros/nyx103
30. Wang M, Wang Z, Ren P, et al. Meningioma with ring enhancement on MRI: a rare case report. BMC Med Imaging. 2021;21:22. doi:10.1186/s12880-021-00555-x
31. Punpichet M, Limcharoenchai C, Suthiwartnaruput K, et al. Internal Cerebral Vein in Susceptibility-Weighted Imaging: A Reliable Tool to Differentiate Among Calcification, Microbleed, and Gross Hemorrhage in Brain Tumors. Cureus. 16(5):e61166. doi:10.7759/cureus.61166
32. Bydder GM, Rutherford MA, Hajnal JV. How to perform diffusion-weighted imaging. Childs Nerv Syst. 2001;17(4-5):195-201. doi:10.1007/s003810000281
33. Albano D, Micci G, Patti C, et al. Whole-Body Magnetic Resonance Imaging: Current Role in Patients with Lymphoma. Diagnostics (Basel). 2021;11(6):1007. doi:10.3390/diagnostics11061007
34. Guo J, Fu X, Li Y, et al. Ultra high b-value diffusion weighted imaging enables better molecular grading stratification over histological grading in adult-type diffuse glioma. Eur J Radiol. 2023;168:111140. doi:10.1016/j.ejrad.2023.111140
35. Kawaji H, Koizumi S, Sakai N, et al. Evaluation of tumor blood flow after feeder embolization in meningiomas by arterial spin-labeling perfusion magnetic resonance imaging. J Neuroradiol. 2013;40(4):303-306. doi:10.1016/j.neurad.2013.04.005
36. Zhao H, Wang HT. Magnetic resonance imaging scanning susceptibility weighted imaging sequences in the diagnosis and prognostic evaluation of neonatal hypoxic-ischemic encephalopathy. World J Clin Cases. 2024;12(17):3012-3018. doi:10.12998/wjcc.v12.i17.3012
37. Wright AM, Wu YC, Feng L, et al. Diffusion magnetic resonance imaging of cerebrospinal fluid dynamics: Current techniques and future advancements. NMR Biomed. 2024;37(9):e5162. doi:10.1002/nbm.5162
38. Rossmeisl JH, Clapp K, Pancotto TE, et al. Canine Butterfly Glioblastomas: A Neuroradiological Review. Front Vet Sci. 2016;3:40. doi:10.3389/fvets.2016.00040
39. Housni A, Boujraf S, Alami B, et al. Assessment of Primary Brain Lymphoma Using Multimodal Magnetic Resonance Imaging and Proton Magnetic Resonance Spectroscopy. Asian J Neurosurg. 2018;13(4):1205-1208. doi:10.4103/ajns.AJNS_137_17
40. Fink KR, Fink JR. Imaging of brain metastases. Surg Neurol Int. 2013;4(Suppl 4):S209-S219. doi:10.4103/2152-7806.111298
41. Luo X, Jiang H, Liu X, et al. Base MRI Imaging Characteristics of Meningioma Patients to Discuss the WHO Classification of Brain Invasion Otherwise Benign Meningiomas. Technol Cancer Res Treat. 2023;22:15330338231171470. doi:10.1177/15330338231171470
42. Zhang S, William C. Educational Case: Histologic and Molecular Features of Diffuse Gliomas. Acad Pathol. 2020;7:2374289520914021. doi:10.1177/2374289520914021
43. Kalode S, Banait S. Radiological and histopathological correlations in oligodendroglioma: a comprehensive case report. Pan Afr Med J. 2024;49:73. doi:10.11604/pamj.2024.49.73.45324
44. Opancina V, Esposito S, Di Meco F, et al. Magnetic resonance imaging characteristics of pediatric pilocytic astrocytoma. Neurol Sci. 2023;44(11):4033-4040. doi:10.1007/s10072-023-06893-8
45. Wagué D, Manneh EK, Sène F, et al. Brain abscess mimicking a brain tumor only realized during surgery: A case report in a resource strained environment. Surg Neurol Int. 2025;16:131. doi:10.25259/SNI_67_2025
46. Dubovoy AV, Jafarov VM, Voronina EI. Supratentorial dural-based collision of cavernoma and meningioma: a case report. Chin Neurosurg J. 2018;4:17. doi:10.1186/s41016-018-0128-5
47. Konar AS, Shah AD, Paudyal R, et al. Quantitative Relaxometry Metrics for Brain Metastases Compared to Normal Tissues: A Pilot MR Fingerprinting Study. Cancers (Basel). 2022;14(22):5606. doi:10.3390/cancers14225606
48. Watanabe H, Arai H, Ogihara K, et al. Diagnostic efficacy of contrast-enhanced fluid-attenuated inversion recovery (FLAIR) imaging in idiopathic cerebrospinal fluid rhinorrhea. Radiol Case Rep. 2024;19(10):4331-4334. doi:10.1016/j.radcr.2024.07.018
49. Raisi-Nafchi M, Faeghi F, Zali A, et al. Preoperative Grading of Astrocytic Supratentorial Brain Tumors with Diffusion-Weighted Magnetic Resonance Imaging and Apparent Diffusion Coefficient. Iran J Radiol. 2016;13(3):e30426. doi:10.5812/iranjradiol.30426
50. Scola E, Desideri I, Bianchi A, et al. Assessment of brain tumors by magnetic resonance dynamic susceptibility contrast perfusion-weighted imaging and computed tomography perfusion: a comparison study. Radiol Med. 2022;127(6):664-672. doi:10.1007/s11547-022-01470-z
51. Booth TC, Wiegers EC, Warnert EAH, et al. High-Grade Glioma Treatment Response Monitoring Biomarkers: A Position Statement on the Evidence Supporting the Use of Advanced MRI Techniques in the Clinic, and the Latest Bench-to-Bedside Developments. Part 2: Spectroscopy, Chemical Exchange Saturation, Multiparametric Imaging, and Radiomics. Frontiers in Oncology. 11(811425). doi:10.3389/fonc.2021.811425
52. Kokkinos V, Chatzisotiriou A, Seimenis I. Functional Magnetic Resonance Imaging and Diffusion Tensor Imaging-Tractography in Resective Brain Surgery: Lesion Coverage Strategies and Patient Outcomes. Brain Sciences. 2023;13(11):1574. doi:10.3390/brainsci13111574
53. Wood J. Private MRI scan costs explained. Practice Plus Group. December 13, 2023. Accessed January 15, 2025. https://practiceplusgroup.com/knowledge-hub/private-mri-scan-costs-explained/