Kidney MRI, also known as renal MRI, utilises powerful magnets, typically with a strength of 1.5 or 3 Tesla, to generate detailed, cross-sectional images of the kidneys, surrounding fat, blood vessels, and the urinary tract. This technique provides exceptional soft-tissue contrast and structural information, making it valuable for both anatomical and functional assessment1,2.
Unlike CT scans, MRI does not use ionising radiation and offers several protocols tailored to patient needs. Multiphasic contrast MRI utilises gadolinium injection to visualise how a tumour enhances or “lights up” helping differentiate benign from malignant lesions3,4. For patients with kidney dysfunction or contrast allergies, non-contrast MRI can be used with core sequences (such as T1, T2, diffusion-weighted, and chemical-shift imaging) without the need for any injection1,5.
Learn more about MRI for cancer detection here.
There are several reasons why a kidney MRI might be ordered, including:
If you have blood in your urine (hematuria) but initial tests, such as ultrasound or CT scans, are unclear or inconclusive, a kidney MRI may be ordered. MRI offers clearer visualisation of the urinary tract and renal tissue, helping to detect tumours, cysts, or subtle structural changes that could be causing the bleeding6,7.
When an unexpected kidney mass is found on a routine scan, an MRI is used to characterise it, such as distinguishing a benign cyst from an angiomyolipoma (AML) or cancer6,7. Its superior soft-tissue contrast helps refine diagnosis and avoid unnecessary surgeries.
In patients already diagnosed with kidney cancer, MRI maps the extent of the tumour, including fat invasion, renal vein and inferior vena cava (IVC) thrombus, lymph node enlargement, and adjacent organ invasion. This precision helps guide surgical and treatment planning6,8.
People with certain hereditary risk factors, such as von Hippel-Lindau syndrome, require lifelong kidney surveillance9. MRI is preferred because it avoids radiation, minimises cumulative risk, and sensitively detects small tumours, cysts, or early-stage cancers that require close monitoring6.
If you have an eGFR below 30 or a history of allergy to iodine-based (CT) or gadolinium-based (MRI) contrast agents, a non-contrast kidney MRI is a safer alternative10,11. Non-contrast MRI provides critical diagnostic information without risking further kidney damage or allergic reactions.
During pregnancy, non-contrast MRI provides a detailed anatomical assessment of the kidneys, urinary tract, and surrounding tissues without the use of ionising radiation or contrast agents. This makes it the safest option when a detailed kidney evaluation is needed for expectant mothers12.
You can use our Know Your Risk Calculator to understand your risk of cancer in just five minutes.
Here are a few tips to help you prepare for your MRI13:
You can read more about preparation for Ezra’s Full Body Scan here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
A kidney MRI scan is a detailed, non-invasive imaging procedure that can be performed with or without the use of contrast. Here’s what you can expect during the scan:
Common Steps (Both Contrast and Non-Contrast Protocols)
Contrast Pathway
If a contrast-enhanced study is needed16:
Non-Contrast Pathway
If no intravenous contrast is given:
Typical Table Time: Expect to spend around 10–15 minutes in the scanner for a non-contrast study and about 25 minutes if contrast is used, depending on the protocol specifics and need for extra imaging.
At Ezra, our Full Body Plus scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
MRI reports for kidney scans often include specialised terms. Here’s a guide to some common phrases and what they mean for your diagnosis:
Ezra provides a radiologist-reviewed report in a non-technical and easy-to-understand format on your dashboard.
After the MRI scan, you will be free to go home and continue with your day without any precautions35. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI precisely measures the tumour’s dimensions and shows its location in relation to the renal hilum (the area where blood vessels, nerves and the ureter connect to the kidney) and nearby vessels36. This spatial accuracy is crucial for determining surgical or interventional strategies.
The way a tumour “lights up” after contrast (enhancement pattern) can hint at its subtype. For instance, clear-cell renal cell carcinomas (RCCs) often exhibit strong, early enhancement, which helps differentiate them from other types, such as papillary or chromophobe RCC37.
Many clear-cell RCCs are surrounded by a thin, dark rim (the pseudocapsule) on MRI. Recognising this sign supports the diagnosis of clear-cell RCC and can guide surgeons toward nephron-sparing procedures38.
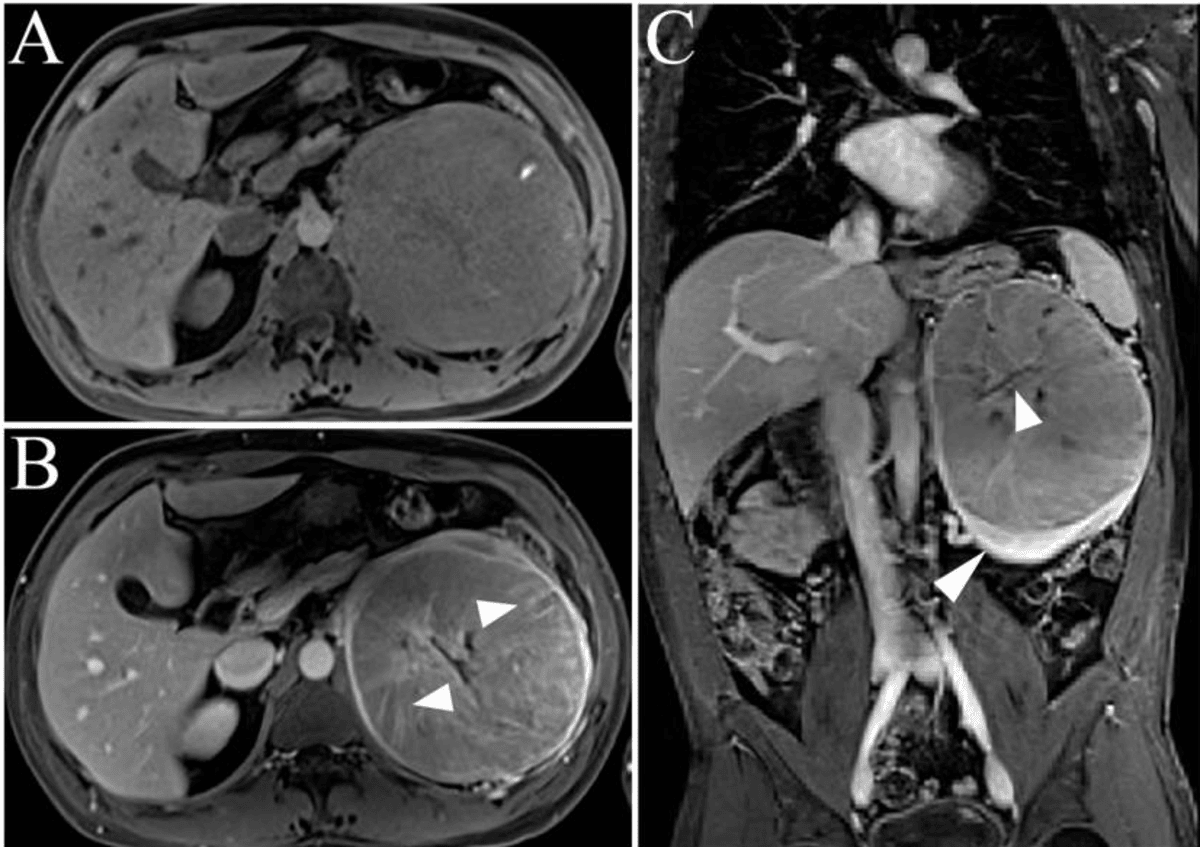
MRI can show the loss of the normal bright fat plane around the kidney, suggesting that the tumour has invaded the surrounding (perinephric) fat36. This finding upstages the disease to at least T3a and has important implications for surgical planning and prognosis.
MRI excels at following tumour-related clot (tumour-thrombus) extending from the renal vein into larger vessels, such as the inferior vena cava (IVC) and even the right atrium of the heart39. Visualising the entire course of such a thrombus is critical for operative strategy and risk assessment.
In a single scan, MRI can also evaluate the lymph nodes and adrenal glands near the kidney. Detecting enlarged or abnormal nodes, or adrenal invasion, influences both staging and the extent of surgery required40.
MRI assesses whether the tumour has come into contact with or invaded organs near the kidney, such as the psoas muscle, colon, or liver41. Involvement of these structures can alter surgical plans, potentially requiring more extensive or multidisciplinary intervention.
Ezra utilises DWI as part of our whole-body MRI scans and artificial intelligence (AI) to enhance MRI images and convert radiology reports into layman's term translations.
Clear-cell renal cell carcinoma (RCC) typically appears very bright on T2-weighted MRI, showing strong, often heterogeneous arterial enhancement after contrast administration42. It also displays low ADC values on diffusion sequences, reflecting its high cellularity. A thin, dark pseudocapsule may also be visible, aiding in the distinction of this aggressive subtype43.
Papillary RCC is characteristically dark on T2-weighted images, demonstrates weak or slow progressive enhancement with gadolinium, and may show high signal intensity on in-phase T1 due to hemosiderin, making it less vascular and distinct from clear-cell RCC44.
Chromophobe RCC shows intermediate signal intensity on T2-weighted MRI, tends to be even in appearance, and enhances moderately and evenly with contrast, generally lacking the strong “wash-in” seen in clear-cell RCC45.
Oncocytoma is a benign tumour that can mimic chromophobe RCC on MRI by showing homogenous enhancement and intermediate to high T2 signal; sometimes, a central stellate scar is present, which is suggestive but not exclusive to oncocytoma46.
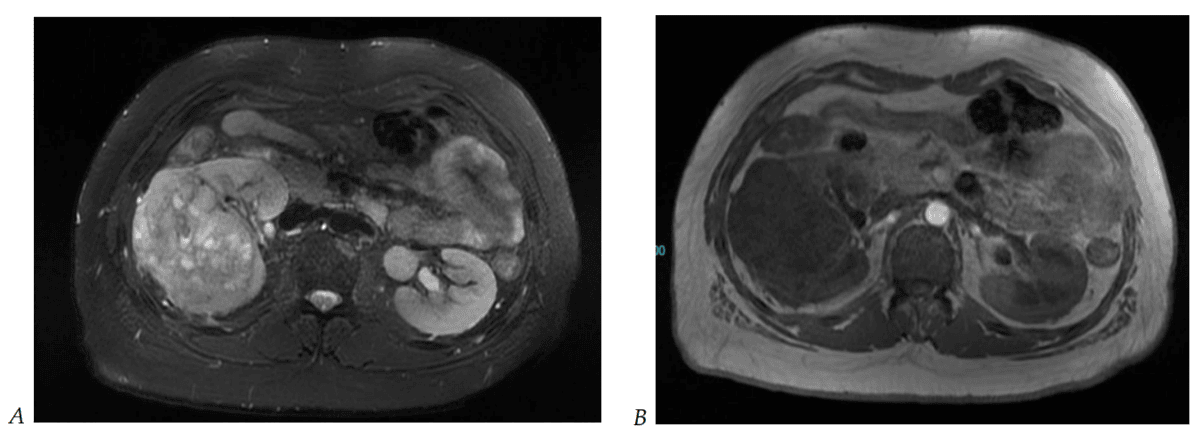
Angiomyolipoma (AML) is identified by signal dropout of macroscopic fat on fat-suppressed T1-weighted images, while classic AMLs appear bright on T2, but fat-poor or hemorrhagic AMLs lack visible fat and may resemble malignant masses47.
Cystic lesions classified as Bosniak II-IV are characterised by complex internal structures, including septations, mural nodules, or irregular walls48. MRI allows for the confident detection of contrast wash-in or enhancement on subtraction images, with Bosniak III/IV cysts carrying a higher malignancy risk.
Wilms tumour, a childhood renal cancer, appears as a large heterogeneous mass that frequently crosses the midline and may displace adjacent organs; MRI is especially useful for follow-up to avoid radiation exposure and can show tumour components such as necrosis or haemorrhage49.
Upper-tract urothelial carcinoma is typically characterised by focal wall thickening or a mass affecting the renal pelvis or ureter, most visible during the delayed (excretory) phase of imaging. MRI can help define the tumour extent and guide surgical management50.
Ezra screens for over 500 conditions, including the kidneys.
There are multiple types of MRI scans, all using different methods to give a better visualisation of kidney tumours.
Ezra uses whole-body DWI imaging to get a full picture of the body and catch any potential abnormalities.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London and in Sidcup, with more locations planned in the future. No referral is required, so you can book your scan directly without first consulting a GP or specialist. Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
For a dedicated kidney MRI, only the part of your body being scanned, typically your abdomen, is placed inside the scanner, not your entire body.
CT scans are generally superior for detecting kidney stones and calcifications, while MRI provides better soft tissue contrast for tumours and is used when avoiding radiation is important.
MRI can sometimes detect kidney stones, but it is much less accurate than CT, which remains the gold standard for identifying stones.



1. Francis ST, Selby NM, Taal MW. Magnetic Resonance Imaging to Evaluate Kidney Structure, Function, and Pathology: Moving Toward Clinical Application. American Journal of Kidney Diseases. 2023;82(4):491-504. doi:10.1053/j.ajkd.2023.02.007
2. Nikken JJ, Krestin GP. MRI of the kidney—state of the art. Eur Radiol. 2007;17(11):2780-2793. doi:10.1007/s00330-007-0701-3
3. Bodard S, Cornelis FH. Non-invasive functional MRI techniques for early detection of kidney injury in chronic kidney disease: a positive step forward. Annals of Translational Medicine. 2024;12(4):80-80. doi:10.21037/atm-23-1788
4. Schieda N, Krishna S, Davenport MS. Update on Gadolinium-Based Contrast Agent–Enhanced Imaging in the Genitourinary System. American Journal of Roentgenology. 2019;212(6):1223-1233. doi:10.2214/AJR.19.21137
5. 3T MR imaging protocol for characterization of renal masses | Applied Radiology. Accessed July 17, 2025. https://appliedradiology.com/articles/3t-mr-imaging-protocol-for-characterization-of-renal-masses
6. Willatt J, Francis IR. Imaging and management of the incidentally discovered renal mass. Cancer Imaging. 2009;9(Special issue A):S30-S37. doi:10.1102/1470-7330.2009.9008
7. Agnello F, Albano D, Micci G, et al. CT and MR imaging of cystic renal lesions. Insights Imaging. 2020;11:5. doi:10.1186/s13244-019-0826-3
8. Reznek RH. CT/MRI in staging renal cell carcinoma. Cancer Imaging. 2004;4(Spec No A):S25-S32. doi:10.1102/1470-7330.2004.0012
9. Ashouri K, Mohseni S, Tourtelot J, et al. Implications of Von Hippel-Lindau Syndrome and Renal Cell Carcinoma. J Kidney Cancer VHL. 2015;2(4):163-173. doi:10.15586/jkcvhl.2015.41
10. Gadolinium contrast injection - Overview. Guy’s and St Thomas’ NHS Foundation Trust. Accessed July 17, 2025. https://www.guysandstthomas.nhs.uk/health-information/gadolinium-contrast-injection
11. Martino F, Amici G, Rosner M, et al. Gadolinium-Based Contrast Media Nephrotoxicity in Kidney Impairment: The Physio-Pathological Conditions for the Perfect Murder. J Clin Med. 2021;10(2):271. doi:10.3390/jcm10020271
12. Gatta G, Di Grezia G, Cuccurullo V, et al. MRI in Pregnancy and Precision Medicine: A Review from Literature. J Pers Med. 2021;12(1):9. doi:10.3390/jpm12010009
13. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
14. Williams JM, Hilmes MA, Archer B, et al. Repeatability and Reproducibility of Pancreas Volume Measurements Using MRI. Sci Rep. 2020;10:4767. doi:10.1038/s41598-020-61759-9
15. Kitazume Y, Satoh S, Taura S, et al. Diffusion-weighted magnetic resonance imaging detection of renal cancer presenting with diffuse peritoneal metastases in a patient with hemodialysis-associated acquired cystic disease of the kidney. J Magn Reson Imaging. 2009;29(4):953-956. doi:10.1002/jmri.21640
16. Thorson D, Bova D, Picken MM, et al. Peak early‐phase enhancement ratio on contrast‐enhanced MRI to differentiate chromophobe renal cell carcinoma from oncocytoma. BJUI Compass. 2025;6(4):e70017. doi:10.1002/bco2.70017
17. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
18. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
19. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
20. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
21. Blum SFU, Ittermann T, Kromrey ML, et al. Long-term outcome of incidental cystic liver tumors in the general population. Sci Rep. 2021;11(1):11661. doi:10.1038/s41598-021-91140-3
22. Moreira-Silva H, Amorim J, Santos-Silva E. Incidental Liver Lesions in children: A practical and evidence-based approach. Clinics and Research in Hepatology and Gastroenterology. 2022;46(5):101904. doi:10.1016/j.clinre.2022.101904
23. Sawatzki M, Husarik DB, Semela D. Assessment of focal liver lesions in non-cirrhotic liver – expert opinion statement by the Swiss Association for the Study of the Liver and the Swiss Society of Gastroenterology. Swiss Medical Weekly. 2023;153(9):40099-40099. doi:10.57187/smw.2023.40099
24. Mall MA, Stahl M, Graeber SY, et al. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
25. Murphy A. CT renal mass (protocol) | Radiology Reference Article | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-94873
26. Themes UFO. Protocol Optimization for Renal Mass Detection and Characterization. Radiology Key. August 15, 2020. Accessed July 17, 2025. https://radiologykey.com/protocol-optimization-for-renal-mass-detection-and-characterization/
27. Yuh BI, Cohan RH. Different phases of renal enhancement: role in detecting and characterizing renal masses during helical CT. AJR Am J Roentgenol. 1999;173(3):747-755. doi:10.2214/ajr.173.3.10470916
28. Grazioli L, Olivetti L, Fugazzola C, et al. The pseudocapsule in hepatocellular carcinoma: correlation between dynamic MR imaging and pathology. Eur Radiol. 1999;9(1):62-67. doi:10.1007/s003300050629
29. Paudyal B, Paudyal P, Tsushima Y, et al. The role of the ADC value in the characterisation of renal carcinoma by diffusion-weighted MRI. Br J Radiol. 2010;83(988):336-343. doi:10.1259/bjr/74949757
30. Bata P, Tarnoki AD, Tarnoki DL, et al. Bosniak category III cysts are more likely to be malignant than we expected in the era of multidetector computed tomography technology. J Res Med Sci. 2014;19(7):634-638.
31. Lam CJ, Kapoor A. The true malignancy risk of Bosniak III cystic renal lesions: Active surveillance or surgical resection? Can Urol Assoc J. 2018;12(6):E276-E280. doi:10.5489/cuaj.4960
32. Kutluhan MA, Ünal S, Eren S, et al. Predictive features of pre-operative computed tomography and magnetic resonance imaging for advanced disease in renal cell carcinoma. Arch Ital Urol Androl. 2022;94(1):1-6. doi:10.4081/aiua.2022.1.1
33. Alayed A, Krishna S, Breau RH, et al. Diagnostic Accuracy of MRI for Detecting Inferior Vena Cava Wall Invasion in Renal Cell Carcinoma Tumor Thrombus Using Quantitative and Subjective Analysis. American Journal of Roentgenology. 2019;212(3):562-569. doi:10.2214/AJR.18.20209
34. Israel GM, Hindman N, Hecht E, et al. The Use of Opposed-Phase Chemical Shift MRI in the Diagnosis of Renal Angiomyolipomas. American Journal of Roentgenology. 2005;184(6):1868-1872. doi:10.2214/ajr.184.6.01841868
35. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
36. Lal H, Singh P, Jain M, et al. Role of MRI in staging and surgical planning and its clinicopathological correlation in patients with renal cell carcinoma. Indian J Radiol Imaging. 2019;29(3):277-283. doi:10.4103/ijri.IJRI_177_19
37. Wang X, Kong W, Wang Y, et al. Analysis of CT, MRI imaging features of renal cell carcinoma with different histopathological types. J BUON. 2021;26(5):2053-2058.
38. Roquero L, Kryvenko ON, Gupta NS, et al. Characterization of Fibromuscular Pseudocapsule in Renal Cell Carcinoma. Int J Surg Pathol. 2015;23(5):359-363. doi:10.1177/1066896915579198
39. Adams LC, Ralla B, Bender YNY, et al. Renal cell carcinoma with venous extension: prediction of inferior vena cava wall invasion by MRI. Cancer Imaging. 2018;18:17. doi:10.1186/s40644-018-0150-z
40. Maatman IT, Schulz J, Ypma S, et al. Free-breathing high-resolution respiratory-gated radial stack-of-stars magnetic resonance imaging of the upper abdomen at 7 T. NMR Biomed. 2024;37(10):e5180. doi:10.1002/nbm.5180
41. Ribeiro SM, Ajzen SA, Trindade JC. [A comparative study of ultrasonography, computed tomography and magnetic resonance imaging in the staging and invasiveness of adjacent structures by renal tumors]. Rev Assoc Med Bras (1992). 2001;47(3):198-207. doi:10.1590/s0104-42302001000300031
42. Halefoglu AM, Ozagari AA. Comparison of cortico-medullary phase contrast-enhanced MDCT and T2-weighted MR imaging in the histological subtype differentiation of renal cell carcinoma: radiology-pathology correlation. Pol J Radiol. 2021;86:e583-e593. doi:10.5114/pjr.2021.111013
43. Zhang HM, Wu YH, Gan Q, et al. Diagnostic Utility of Diffusion-weighted Magnetic Resonance Imaging in Differentiating Small Solid Renal Tumors (≤4 cm) at 3.0T Magnetic Resonance Imaging. Chin Med J (Engl). 2015;128(11):1444-1449. doi:10.4103/0366-6999.157648
44. Nalbant MO, Inci E. Assessment of Imaging Findings of Renal Carcinoma Subtypes with 3.0T MRI. Nigerian Journal of Clinical Practice. 2023;26(11):1750. doi:10.4103/njcp.njcp_373_23
45. Chartier S, Arif-Tiwari H. MR Virtual Biopsy of Solid Renal Masses: An Algorithmic Approach. Cancers (Basel). 2023;15(10):2799. doi:10.3390/cancers15102799
46. Trevisani F, Floris M, Minnei R, et al. Renal Oncocytoma: The Diagnostic Challenge to Unmask the Double of Renal Cancer. Int J Mol Sci. 2022;23(5):2603. doi:10.3390/ijms23052603
47. Labra A, Schiappacasse G, Constenla D, et al. Renal angiomyolipomas: Typical and atypical features on computed tomography and magnetic resonance imaging. World J Radiol. 2025;17(2):104282. doi:10.4329/wjr.v17.i2.104282
48. Chan J, Yan JH, Munir J, et al. Comparison of Bosniak Classification of cystic renal masses version 2019 assessed by CT and MRI. Abdom Radiol (NY). 2021;46(11):5268-5276. doi:10.1007/s00261-021-03236-z
49. Belt TG, Cohen MD, Smith JA, et al. MRI of Wilms’ tumor: promise as the primary imaging method. AJR Am J Roentgenol. 1986;146(5):955-961. doi:10.2214/ajr.146.5.955
50. Froemming A, Potretzke T, Takahashi N, et al. Upper tract urothelial cancer. Eur J Radiol. 2018;98:50-60. doi:10.1016/j.ejrad.2017.10.021
51. Zheng L, Yang C, Sheng R, et al. Renal imaging at 5 T versus 3 T: a comparison study. Insights Imaging. 2022;13:155. doi:10.1186/s13244-022-01290-9
52. de Silva S, Lockhart KR, Aslan P, et al. Differentiation of renal masses with multi-parametric MRI: the de Silva St George classification scheme. BMC Urol. 2022;22:141. doi:10.1186/s12894-022-01082-9
53. Sweis RF, Medved M, Towey S, et al. Dynamic Contrast Enhanced-Magnetic Resonance Imaging as a Pharmacodynamic Biomarker for Pazopanib in Metastatic Renal Carcinoma. Clin Genitourin Cancer. 2017;15(2):207-212. doi:10.1016/j.clgc.2016.08.011
54. Wang H yi, Su Z hua, Xu X, et al. Dynamic Contrast-enhanced MR Imaging in Renal Cell Carcinoma: Reproducibility of Histogram Analysis on Pharmacokinetic Parameters. Sci Rep. 2016;6(1):29146. doi:10.1038/srep29146
55. de Silva S, Lockhart KR, Aslan P, et al. The diagnostic utility of diffusion weighted MRI imaging and ADC ratio to distinguish benign from malignant renal masses: sorting the kittens from the tigers. BMC Urol. 2021;21:67. doi:10.1186/s12894-021-00832-5
56. Meena JK, Taneja A. Role of diffusion: weighted magnetic resonance imaging in evaluation of renal masses. International Journal of Research in Medical Sciences. 2020;8(10):3575-3584. doi:10.18203/2320-6012.ijrms20204232
57. Maj E, Cieszanowski A, Rowiński O, et al. Time-resolved contrast-enhanced MR angiography: Value of hemodynamic information in the assessment of vascular diseases. Pol J Radiol. 2010;75(1):52-60.
58. Robson PM, Madhuranthakam AJ, Smith MP, et al. Volumetric Arterial Spin Labeled Perfusion Imaging Of The Kidneys with a Three Dimensional Fast Spin Echo Acquisition. Acad Radiol. 2016;23(2):144-154. doi:10.1016/j.acra.2015.09.013
59. Pagé G, Garteiser P, Van Beers BE. Magnetic resonance elastography of malignant tumors. Front Phys. 2022;10. doi:10.3389/fphy.2022.910036
60. Zhang HM, Wen DG, Chen J, et al. A diagnostic test of three-dimensional magnetic resonance elastography imaging for preoperative prediction of microvascular invasion in patients with T1 stage clear cell renal carcinoma. Translational Andrology and Urology. 2023;12(3):46676-46476. doi:10.21037/tau-23-94