Pancreatic cancer is often symptomless until it reaches advanced stages (III-IV), making early diagnosis rare and prognosis poor. In the UK, fewer than 10 per cent of patients are eligible for potentially curative surgery at diagnosis, and overall five-year survival remains below 7 per cent1,2. However, if a tumour is detected when it is 2 cm or smaller and surgery is possible, five-year survival can increase dramatically to over 40 per cent.
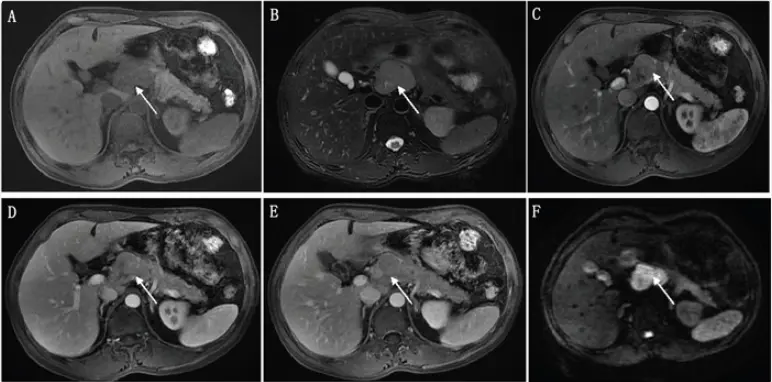
Advanced imaging, particularly MRI combined with MRCP (magnetic resonance cholangiopancreatography) and diffusion-weighted techniques, offers a crucial advantage in early detection3. It demonstrates high sensitivity and accuracy in detecting pancreatic tumours, comparable to computed tomography4.
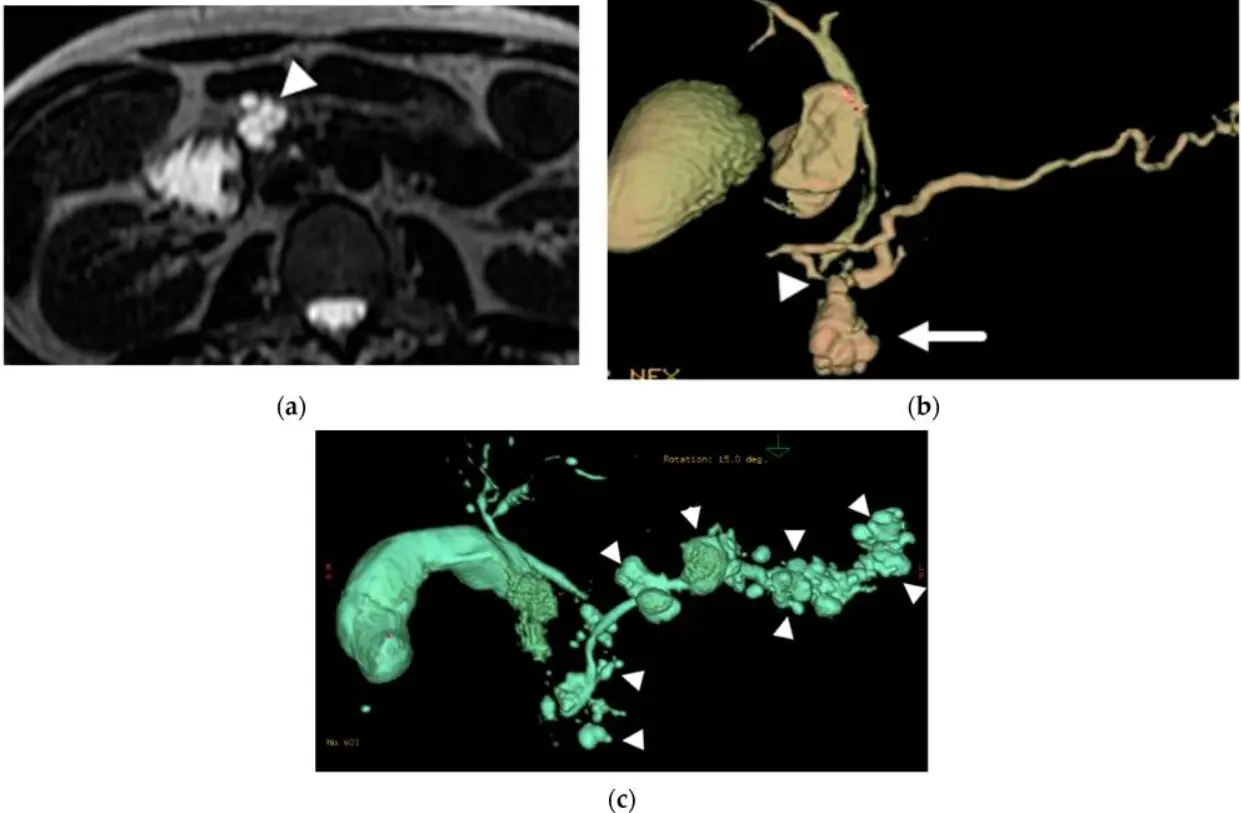
Early MRI-based detection also enables the identification of precursor lesions, such as high-risk intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms5. Resection of these lesions before they become invasive provides a unique opportunity to prevent pancreatic cancer altogether, highlighting the critical role of advanced imaging in improving outcomes for UK patients.
Learn more about MRI for cancer detection here.
There are several reasons why a pancreas MRI might be ordered, including:
Here are a few tips to help you prepare for your MRI16:
You can read more about preparation for Ezra’s Full Body Scan here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the scan, you will lie down on a sliding table. A dedicated surface or phased-array coil is typically placed over the limb or region of interest18. Your head will be nestled in a small cushion that will keep you still. The scan typically lasts 30-45 minutes of actual “table time”, during which the technician may acquire multiple sequences (settings), including T1-, T2-, and DWI/ADC weighted images, and often MRCP sequences to visualise the pancreatic and bile ducts in detail19,20. Other sequences that can be included are fat-suppressed T1-weighted imaging, elastography, secretin-enhanced MRCP, and extracellular volume quantification.
You may be asked to hold your breath for short periods during the scan to minimise motion and improve image clarity.
You may also be given pineapple juice or ferumoxsil, which act as negative contrast agents to improve the visibility of the bile and pancreatic ducts21,22.
You’ll hear a series of loud knocking or tapping sounds as the MRI machine works. This is completely normal. The scan usually takes about 20 to 45 minutes, and you’ll be offered earplugs or headphones to make the experience more comfortable.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the coil is removed, and you’re free to go.
At Ezra, our Full Body Plus scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
MRI reports for the pancreas often use technical language. Here’s a guide to some common terms and what they mean for your diagnosis and treatment:
Ezra provides a radiologist-reviewed report in a non-technical and easy-to-understand format on your dashboard.
After the MRI scan, you will be free to go home and continue with your day without any precautions38. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI provides highly detailed images, allowing radiologists to measure the size and pinpoint the precise location of a pancreatic tumour down to the millimetre. This accuracy is crucial for surgical planning and assessing whether the tumour is operable39.
MRI can reveal if the tumour has invaded nearby blood vessels, such as the superior mesenteric artery (SMA) or portal vein40. If the tumour wraps around these vessels by 180° or more, surgery may require vascular grafting or may be contraindicated altogether, as this degree of invasion often means the cancer is unresectable.
Using MRCP sequences, MRI can assess the calibre of the pancreatic and bile ducts, detect abrupt ductal cut-offs (which can indicate tumour location), and identify side-branch communications37,41. These findings help diagnose and characterise both cancer and its precursor lesions.
MRI with diffusion-weighted imaging can show areas where water movement is restricted and provide apparent diffusion coefficient (ADC) values31. Low ADC values often correlate with high tumour cellularity and aggressiveness, helping to distinguish malignant from benign tissue.
MRI is sensitive for detecting enlarged or abnormal lymph nodes around the pancreas and can identify subtle liver or peritoneal metastases that may not be visible on CT scans42. This ability is vital for accurate staging and treatment planning.
MRI can visualise tumour spread along the celiac or SMA nerve plexuses43. Detecting neural invasion is important because it increases the risk of local recurrence after treatment and may influence surgical decision-making.
Ezra utilises DWI as part of our whole-body MRI scans and artificial intelligence (AI) to enhance MRI images and convert radiology reports into layman's term translations.
Ezra screens for over 500 conditions and 13 organs, including pancreas.
There are multiple types of MRI scans, all using different methods to give a better visualisation of pancreatic tumours.
Ezra uses whole-body DWI imaging to get a full picture of the body and catch any potential abnormalities.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London and in Sidcup, with more locations planned in the future. No referral is required, so you can book your scan directly without consulting a GP or specialist first. Most people pay out of pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
Yes, MRI can occasionally miss very small tumours or those that closely mimic benign changes, especially in early or subtle changes.
MRI is highly sensitive but a definitive diagnosis usually requires a tissue biopsy in addition to imaging.
MRCP is a specialised MRI technique focused on imaging the pancreatic and bile ducts, while standard MRI provides broader information about the pancreas and surrounding tissues; both are often used together for a comprehensive assessment.
MRCP is non-invasive and excellent for visualising ducts, but ERCP allows for direct intervention and biopsy, though it carries more risk.
Ready to take proactive steps for your health? Book an Ezra full-body MRI today to detect any issues early and put you on the road to long-term health. Our yearly scan screens for potential cancers early, using AI to enhance the process, making it more efficient and affordable.



1. Pancreatic cancer statistics. Pancreatic Cancer UK. Accessed July 10, 2025. https://www.pancreaticcancer.org.uk/what-we-do/media-centre/pancreatic-cancer-statistics/
2. Action PC. Pancreatic Cancer Prognosis & Survival | Pancreatic Cancer Awareness |. Pancreatic Cancer Action. Accessed July 10, 2025. https://pancreaticcanceraction.org/about-pancreatic-cancer/pancreatic-cancer-prognosis-and-survival/
3. Radiology (ACR) RS of NA (RSNA) and AC of. MRCP (MR Cholangiopancreatography). Radiologyinfo.org. Accessed July 10, 2025. https://www.radiologyinfo.org/en/info/mrcp
4. Chu LC, Goggins MG, Fishman EK. Diagnosis and Detection of Pancreatic Cancer. Cancer J. 2017;23(6):333-342. doi:10.1097/PPO.0000000000000290
5. Flammia F, Fusco R, Triggiani S, et al. Risk Assessment and Radiomics Analysis in Magnetic Resonance Imaging of Pancreatic Intraductal Papillary Mucinous Neoplasms (IPMN). Cancer Control. 2024;31:10732748241263644. doi:10.1177/10732748241263644
6. Schaible J, Grenacher L, Stroszczynski C, et al. The chronic pancreatitis (CP) Type Cambridge 2 as a cause of unclear upper abdominal pain: a radiologically underestimated diagnosis. Rofo. 2024;196(12):1262-1269. doi:10.1055/a-2275-0946
7. Frank RC, Shim B, Lo T, et al. Pancreatic Cancer Screening in New-onset and Deteriorating Diabetes: Preliminary Results From the PANDOME Study. The Journal of Clinical Endocrinology & Metabolism. Published online May 29, 2025:dgaf319. doi:10.1210/clinem/dgaf319
8. Pannala R, Basu A, Petersen GM, et al. New-onset Diabetes: A Potential Clue to the Early Diagnosis of Pancreatic Cancer. Lancet Oncol. 2009;10(1):88-95. doi:10.1016/S1470-2045(08)70337-1
9. Krishna N, Tummala P, Reddy AV, et al. Dilation of both pancreatic duct and the common bile duct on computed tomography and magnetic resonance imaging scans in patients with or without obstructive jaundice. Pancreas. 2012;41(5):767-772. doi:10.1097/MPA.0b013e31823ba536
10. Lowe T, Deluca J, Abenavoli L, et al. Pancreatic Cancer and the Family Connection: The Role of Advanced Practitioners in Screening and Educating Genetically At-Risk Individuals. J Adv Pract Oncol. 2023;14(6):533-539. doi:10.6004/jadpro.2023.14.6.6
11. Welinsky S, Lucas AL. Familial Pancreatic Cancer and the Future of Directed Screening. Gut Liver. 2017;11(6):761-770. doi:10.5009/gnl16414
12. Overbeek KA, Levink IJM, Koopmann BDM, et al. Long-term yield of pancreatic cancer surveillance in high-risk individuals. Gut. 2022;71(6):1152-1160. doi:10.1136/gutjnl-2020-323611
13. Halankar J, Jhaveri K, Metser U. Cystic lesions of the pancreatico-biliary tree: A schematic MRI approach. Indian J Radiol Imaging. 2017;27(2):167-176. doi:10.4103/ijri.IJRI_226_16
14. Hussien N, Hussien RS, Saad DHA, et al. The Role of MRI Pancreatic Protocol in Assessing Response to Neoadjuvant Therapy for Patients With Borderline Resectable Pancreatic Cancer. Front Oncol. 2022;11:796317. doi:10.3389/fonc.2021.796317
15. Zhang Y, Huang ZX, Song B. Role of imaging in evaluating the response after neoadjuvant treatment for pancreatic ductal adenocarcinoma. World J Gastroenterol. 2021;27(22):3037-3049. doi:10.3748/wjg.v27.i22.3037
16. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
17. Williams JM, Hilmes MA, Archer B, et al. Repeatability and Reproducibility of Pancreas Volume Measurements Using MRI. Sci Rep. 2020;10:4767. doi:10.1038/s41598-020-61759-9
18. Gruber B, Froeling M, Leiner T, et al. RF coils: A practical guide for nonphysicists. J Magn Reson Imaging. 2018;48(3):590-604. doi:10.1002/jmri.26187
19. Sandrasegaran K, Lin C, Akisik FM, et al. State-of-the-Art Pancreatic MRI. American Journal of Roentgenology. 2010;195(1):42-53. doi:10.2214/AJR.10.4421
20. Hill DV, Tirkes T. Advanced MR Imaging of the Pancreas. Magn Reson Imaging Clin N Am. 2020;28(3):353-367. doi:10.1016/j.mric.2020.03.003
21. Leung K. Ferumoxsil. In: Molecular Imaging and Contrast Agent Database (MICAD). National Center for Biotechnology Information (US); 2004. Accessed July 10, 2025. http://www.ncbi.nlm.nih.gov/books/NBK22994/
22. Mohabir S, Pitcher RD, Perumal R, et al. The efficacy of pineapple juice as a negative oral contrast agent in magnetic resonance cholangiopancreatography. SA J Radiol. 2020;24(1):1875. doi:10.4102/sajr.v24i1.1875
23. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
24. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
25. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
26. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
27. Gore RM, Wenzke DR, Thakrar KH, et al. The incidental cystic pancreas mass: a practical approach. Cancer Imaging. 2012;12(2):414-421. doi:10.1102/1470-7330.2012.9054
28. Kruse E D, Paulson E K. The Incidental Pancreatic Cyst: When to Worry About Cancer. Korean Journal of Radiology. 2024;25(6):559-564. doi:10.3348/kjr.2024.0085
29. Mall MA, Stahl M, Graeber SY, et al. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
30. Miller FH, Lopes Vendrami C, Hammond NA, et al. Pancreatic Cancer and Its Mimics. RadioGraphics. 2023;43(11):e230054. doi:10.1148/rg.230054
31. Abdelgawad EA, Rahim AMA, Rahman A shimaa MA. Can diffusion-weighted MRI replace conventional contrast enhanced MRI in the differentiation between benign and malignant pancreatic masses? The Egyptian Journal of Radiology and Nuclear Medicine. 2018;49(4):899-902. doi:10.1016/j.ejrnm.2018.07.014
32. Oterdoom LH, van Weyenberg SJB, de Boer NKH. Double-duct sign: do not forget the gallstones. J Gastrointestin Liver Dis. 2013;22(4):447-450.
33. Mullapudi B, Hawkes PJ, Patel A, et al. Borderline Resectable Pancreatic Cancer. Indian J Surg Oncol. 2015;6(1):63-68. doi:10.1007/s13193-014-0374-8
34. Levy MJ, Topazian M, Keeney G, et al. Preoperative Diagnosis of Extrapancreatic Neural Invasion in Pancreatic Cancer. Clinical Gastroenterology and Hepatology. 2006;4(12):1479-1482. doi:10.1016/j.cgh.2006.08.012
35. Boraschi P, Tarantini G, Donati F, et al. Side-branch intraductal papillary mucinous neoplasms of the pancreas: outcome of MR imaging surveillance over a 10 years follow-up. Eur J Radiol Open. 2020;7:100250. doi:10.1016/j.ejro.2020.100250
36. Zhong N, Zhang L, Takahashi N, et al. Histologic and Imaging Features of Mural Nodules in Mucinous Pancreatic Cysts. Clinical Gastroenterology and Hepatology. 2012;10(2):192-198.e2. doi:10.1016/j.cgh.2011.09.029
37. Johnston A, Serhal A, Lopes Vendrami C, et al. The abrupt pancreatic duct cutoff sign on MDCT and MRI. Abdom Radiol (NY). 2020;45(8):2476-2484. doi:10.1007/s00261-020-02582-8
38. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
39. Michallek F, Haouari MA, Dana O, et al. Fractal analysis improves tumour size measurement on computed tomography in pancreatic ductal adenocarcinoma: comparison with gross pathology and multi-parametric MRI. Eur Radiol. 2022;32(8):5053-5063. doi:10.1007/s00330-022-08631-8
40. Zhou X, Xu D, Wang M, et al. Preoperative assessment of peripheral vascular invasion of pancreatic ductal adenocarcinoma based on high-resolution MRI. BMC Cancer. 2023;23:1092. doi:10.1186/s12885-023-11451-8
41. Balcı C. MRI assessment of chronic pancreatitis. Diagn Interv Radiol. 2011;17(3):249-254. doi:10.4261/1305-3825.DIR.3889-10.0
42. Luo YG, Wu M, Chen HG. Retrospective analysis of pathological types and imaging features in pancreatic cancer: A comprehensive study. World J Gastrointest Oncol. 2025;17(1):99153. doi:10.4251/wjgo.v17.i1.99153
43. Liu YL, Zhu HB, Chen ML, et al. Prediction of the lymphatic, microvascular, and perineural invasion of pancreatic neuroendocrine tumors using preoperative magnetic resonance imaging. World J Gastrointest Surg. 2023;15(12):2809-2819. doi:10.4240/wjgs.v15.i12.2809
44. Miller FH, Rini NJ, Keppke AL. MRI of Adenocarcinoma of the Pancreas. American Journal of Roentgenology. 2006;187(4):W365-W374. doi:10.2214/AJR.05.0875
45. Guo C, Chen X, Wang Z, et al. Differentiation of pancreatic neuroendocrine carcinoma from pancreatic ductal adenocarcinoma using magnetic resonance imaging: The value of contrast-enhanced and diffusion weighted imaging. Oncotarget. 2017;8(26):42962-42973. doi:10.18632/oncotarget.17309
46. Manfredi R, Bonatti M, Mantovani W, et al. Non-hyperfunctioning neuroendocrine tumours of the pancreas: MR imaging appearance and correlation with their biological behaviour. Eur Radiol. 2013;23(11):3029-3039. doi:10.1007/s00330-013-2929-4
47. Hu F, Hu Y, Wang D, et al. Cystic Neoplasms of the Pancreas: Differential Diagnosis and Radiology Correlation. Front Oncol. 2022;12:860740. doi:10.3389/fonc.2022.860740
48. Roalsø MTT, Hughes DL, Larsson P, et al. Mucinous cystic neoplasia (MCN) of the pancreas: systematic review and meta-analysis of sex differences in prevalence and malignancy risk between males and females. Chin Clin Oncol. 2025;14(2):19. doi:10.21037/cco-24-124
49. Quingalahua E, Al-Hawary MM, Machicado JD. The Role of Magnetic Resonance Imaging (MRI) in the Diagnosis of Pancreatic Cystic Lesions (PCLs). Diagnostics (Basel). 2023;13(4):585. doi:10.3390/diagnostics13040585
50. Kovac JD, Djikic-Rom A, Bogdanovic A, et al. The Role of MRI in the Diagnosis of Solid Pseudopapillary Neoplasm of the Pancreas and Its Mimickers: A Case-Based Review with Emphasis on Differential Diagnosis. Diagnostics (Basel). 2023;13(6):1074. doi:10.3390/diagnostics13061074
51. Wu J, Mao Y, Jiang Y, et al. Sex differences in solid pseudopapillary neoplasm of the pancreas: A population‐based study. Cancer Med. 2020;9(16):6030-6041. doi:10.1002/cam4.3180
52. Sikka A, Adam SZ, Wood C, et al. Magnetic resonance imaging of pancreatic metastases from renal cell carcinoma. Clinical Imaging. 2015;39(6):945-953. doi:10.1016/j.clinimag.2015.07.012
53. Zhang XM, Mitchell DG, Dohke M, et al. Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology. 2002;223(2):547-553. doi:10.1148/radiol.2232010815
54. ŞAHAN MH, ÖZDEMİR A, ASAL N, et al. Pancreas and kidney changes in type 2 diabetes patients: the role of diffusion-weighted imaging. Turk J Med Sci. 2021;51(3):1289-1295. doi:10.3906/sag-2011-176
55. Zhang T, Shi X, Li J, et al. Horizontal duodenal papilla is associated with a special spectrum of pancreaticobiliary diseases: a retrospective magnetic resonance cholangiopancreatography-based study. Gastroenterol Rep (Oxf). 2024;12:goae059. doi:10.1093/gastro/goae059
56. Sanyal R, Stevens T, Novak E, et al. Secretin-enhanced MRCP: review of technique and application with proposal for quantification of exocrine function. AJR Am J Roentgenol. 2012;198(1):124-132. doi:10.2214/AJR.10.5713
57. Liu X, Wang YF, Qi XH, et al. Reproducibility study of intravoxel incoherent motion and apparent diffusion coefficient parameters in normal pancreas. World J Gastrointest Surg. 2024;16(7):2031-2039. doi:10.4240/wjgs.v16.i7.2031
58. Steinkohl E, Bertoli D, Hansen TM, et al. Practical and clinical applications of pancreatic magnetic resonance elastography: a systematic review. Abdom Radiol (NY). 2021;46(10):4744-4764. doi:10.1007/s00261-021-03143-3