A uterine magnetic resonance imaging (MRI) scan is a safe and non-invasive imaging technique that provides high-resolution images of the uterus and surrounding tissues, making it the preferred method for diagnosing and staging uterine cancers, such as endometrial carcinoma and uterine sarcomas. This advanced imaging test accurately determines tumour size, depth of invasion, and involvement of pelvic structures, supporting effective treatment planning and prognosis assessment1,2.
MRI surpasses other imaging modalities in soft-tissue contrast and staging accuracy, offering valuable information for both surgical and non-surgical management decisions. Its use is essential in guiding the multidisciplinary care of patients suspected of or diagnosed with uterine cancer.
A uterine MRI might be recommended for several reasons:
Here are a few tips to help you prepare for your MRI8:
You can read more about preparation for Ezra’s MRI Scan with Spine here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the scan, you will lie down on a sliding table. A dedicated surface or phased-array coil is typically placed over the limb or region of interest9. Your head will be nestled in a small cushion that will keep you still. The scan typically lasts 30-45 minutes of actual “table time”, during which the technician may acquire multiple sequences (settings). Expect loud knocking noises (up to 110 dB); earplugs or headphones are provided to reduce discomfort. It’s normal to feel mild table vibrations.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the coil is removed, and you’re free to go.
At Ezra, our MRI Scan with Spine scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
After the scan, you will be contacted by a medical provider working with Ezra within roughly a week. On the day of the appointment, you will receive a copy of your report and access to your scanned images through the online portal.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
MRI reports of the uterus include specific terms that help clinicians assess the nature of a lesion or condition. Some common terms (and their meaning) include:
Myometrial Invasion: This refers to how deeply a tumour has invaded into the muscle wall (the myometrium) of the uterus16. Less than 50 per cent invasion is considered superficial (lower risk), while 50 per cent or more is “deep” invasion (higher risk for recurrence and nodal metastasis)17. Myometrial invasion extent helps determine FIGO stage I subcategories.
Cervical Stromal Invasion: Indicates tumour spread into the fibrous tissue (“stroma”) of the cervix. This upstages the disease to at least FIGO stage II18. On MRI, disruption of the normal low signal in the cervical stroma on T2-weighted imaging suggests such invasion.
Restricted Diffusion/Low ADC: Refers to the reduced motion of water molecules detected on diffusion-weighted imaging (DWI)19. Tumours with high cellular density (often aggressive) demonstrate restricted diffusion and low apparent diffusion coefficient (ADC) values. This finding can help identify more aggressive subtypes.
Serosal Involvement: Implies the tumour has invaded through the uterine wall to the serosal (outermost) surface or beyond20. This finding changes the disease stage to IIIA and denotes local extension outside the uterus.
T2 Signal Intensity: On MRI, T2 signal intensity helps characterise tissues based on water content and cellular structure21. Tumours may appear with a varied T2 signal compared to normal uterine tissue, aiding in identifying myometrial or cervical invasion.
Lymphadenopathy: Describes lymph nodes that are enlarged or appear suspicious for malignancy on imaging22. Lymphadenopathy can indicate possible regional (pelvic/para-aortic) lymph node metastasis, which upstages the disease to IIIC23.
After the MRI scan, you will be free to go home and continue with your day without any precautions24. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol, or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI can provide comprehensive information about uterine cancer, aiding diagnosis, staging, and treatment monitoring.
MRI provides precise visualisation of the tumour within the uterine cavity, accurately measures its dimension (within 0.5 cm of surgical size in up to 90 per cent of cases), and localises it in relation to key uterine structures1.
MRI is considered the best tool for assessing how deeply the tumour has invaded the myometrium. This is highly predictive of risk. The deeper the invasion, the higher the risk of lymphatic spread and recurrence1.
MRI can identify cervical stromal invasion (accuracy up to 92 per cent), serosal involvement, and direct extension into surrounding pelvic tissues or organs such as the vagina, bladder, or rectum1,2.
MRI visualises pelvic, para-aortic, and inguinal (groin) lymphadenopathy and can suggest metastatic disease, especially if nodes show central necrosis2.
MRI can show the size, location, and texture of a uterine tumour, and highlight differences within the tumour itself25. These details help doctors predict how aggressive the cancer might be by looking at patterns inside the tumour and how it appears on different types of MRI images. Some features, like certain brightness or dark areas, may suggest a faster-growing or higher-grade cancer.
MRI helps doctors distinguish between different types of uterine tumours by showing their size, shape, and how they interact with nearby tissues.
This cancer grows from the lining of the uterus. On MRI, it often looks like a mass with medium brightness and can show spreading into the muscle wall26.

This is a rare cancer of the muscle layer. This type shows up as a large, uneven mass that may contain spots of dead tissue (necrosis) and looks very mixed or “patchy” on scans27.
This less common cancer tends to weave into the tissues and vessels around the uterus, with fuzzy borders and a brighter appearance on certain MRI images28.
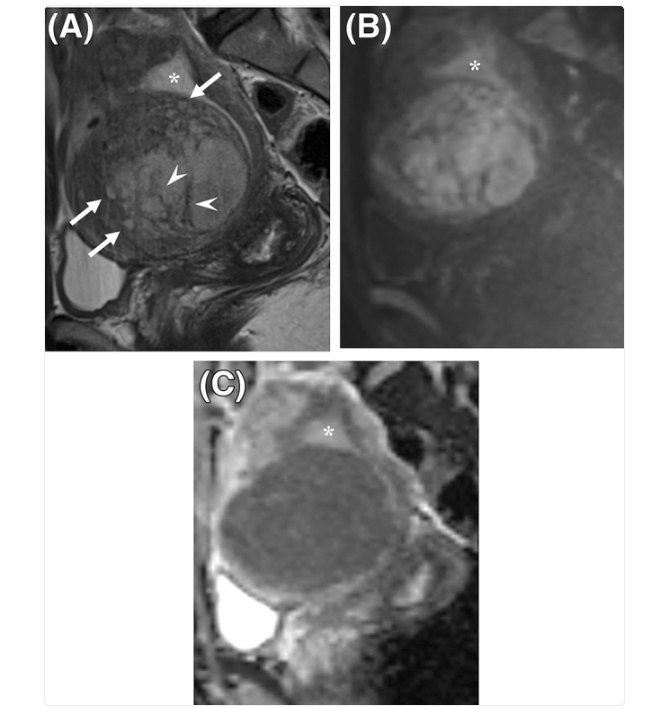
The most common non-cancerous growth, which shows up as a well-shaped, dark mass that doesn’t invade surrounding tissue28,30.
Ezra screens for over 500 conditions, including the brain.
Radiologists use several types of MRI scans to help detect and evaluate uterine cancer. Each scan type offers unique information about the tumour and surrounding tissues:
Highlights the difference between the tumour and normal uterus muscle, helping to map how far the cancer has spread31.
DWI shows how tightly packed tumour cells are. Cancer cells restrict the movement of water, which stands out on this scan32.
Measures water movement in tissue. Lower ADC values usually mean a more aggressive cancer, because the cells are densely packed33.
Involves injecting a contrast dye and tracking how quickly the tumour absorbs it. Aggressive cancers often take up contrast faster and in different ways, guiding assessment of the tumour’s blood supply and spread34.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London, and in Sidcup, with more locations planned in the future. No referral is required, so you can book your scan directly without consulting a GP or specialist first. Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
No, the scan itself is painless, although lying still may be slightly uncomfortable.
You do not always need contrast dye. Ezra offers a contrast-free scan.
No. MRI helps with staging and surgical planning, but biopsy confirms the diagnosis.
MRI provides more detailed images, especially for assessing tumour spread. Ultrasound is still useful as an initial test.



1. Sala E, Wakely S, Senior E, Lomas D. MRI of Malignant Neoplasms of the Uterine Corpus and Cervix. American Journal of Roentgenology. 2007;188(6):1577-1587. doi:10.2214/AJR.06.1196
2. Rizescu RA, Sălcianu IA, Șerbănoiu A, et al. Can MRI Accurately Diagnose and Stage Endometrial Adenocarcinoma? Medicina (Kaunas). 2024;60(3):512. doi:10.3390/medicina60030512
3. Pintican R, Bura V, Zerunian M, et al. MRI of the endometrium - from normal appearances to rare pathology. Br J Radiol. 2021;94(1125):20201347. doi:10.1259/bjr.20201347
4. Uhasai K, Naik D, P R. Efficacy of MRI Over Ultrasound in Evaluation of Abnormal Uterine Bleeding With Histopathological Correlation. Cureus. 15(5):e38560. doi:10.7759/cureus.38560
5. Cardia PP. Indications for magnetic resonance imaging of the female pelvis at a referral center for cancer. Radiol Bras. 2017;50(1):V-VI. doi:10.1590/0100-3984.2017.50.1e1
6. Kubik-Huch RA, Weston M, Nougaret S, et al. European Society of Urogenital Radiology (ESUR) Guidelines: MR Imaging of Leiomyomas. Eur Radiol. 2018;28(8):3125-3137. doi:10.1007/s00330-017-5157-5
7. Kierans AS, Bennett GL, Haghighi M, Rosenkrantz AB. Utility of conventional and diffusion-weighted MRI features in distinguishing benign from malignant endometrial lesions. Eur J Radiol. 2014;83(4):726-732. doi:10.1016/j.ejrad.2013.11.030
8. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
9. Gruber B, Froeling M, Leiner T, Klomp DWJ. RF coils: A practical guide for nonphysicists. J Magn Reson Imaging. 2018;48(3):590-604. doi:10.1002/jmri.26187
10. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
11. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
12. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
13. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
14. Ouldamer L, Rossard L, Arbion F, Marret H, Body G. Risk of Incidental Finding of Endometrial Cancer at the Time of Hysterectomy for Benign Condition. Journal of Minimally Invasive Gynecology. 2014;21(1):131-135. doi:10.1016/j.jmig.2013.08.002
15. Mall MA, Stahl M, Graeber SY, Sommerburg O, Kauczor HU, Wielpütz MO. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
16. cancer CCS/ S canadienne du. Prognosis and survival for uterine cancer. Canadian Cancer Society. Accessed February 21, 2025. https://cancer.ca/en/cancer-information/cancer-types/uterine/prognosis-and-survival
17. Dane C, Bakir S. The effect of myometrial invasion on prognostic factors and survival analysis in endometrial carcinoma. Afr Health Sci. 2019;19(4):3235-3241. doi:10.4314/ahs.v19i4.47
18. Menendez-Santos M, Gonzalez-Baerga C, Taher D, Waters R, Virarkar M, Bhosale P. Endometrial Cancer: 2023 Revised FIGO Staging System and the Role of Imaging. Cancers (Basel). 2024;16(10):1869. doi:10.3390/cancers16101869
19. Baliyan V, Das CJ, Sharma R, Gupta AK. Diffusion weighted imaging: Technique and applications. World J Radiol. 2016;8(9):785-798. doi:10.4329/wjr.v8.i9.785
20. Jobsen JJ, Naudin ten Cate L, Lybeert MLM, et al. Outcome of Endometrial Cancer Stage IIIA with Adnexa or Serosal Involvement Only. Obstet Gynecol Int. 2011;2011:962518. doi:10.1155/2011/962518
21. Xu H, Zhang J, Han Y, et al. Role of T2 mapping of magnetic resonance imaging in the differentiation of endometrial cancer and benign endometrial lesions. Diagn Interv Radiol. 2023;29(1):183-189. doi:10.4274/dir.2021.21884
22. Unexplained Lymphadenopathy: Evaluation and Differential Diagnosis | AAFP. Accessed November 19, 2025. https://www.aafp.org/pubs/afp/issues/2016/1201/p896.html
23. Womb cancer and the lymphatic system - Macmillan Cancer Support. Accessed November 19, 2025. https://www.macmillan.org.uk/cancer-information-and-support/womb-cancer/womb-cancer-and-the-lymphatic-system
24. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
25. Kumagai K, Yagi T, Yamazaki M, Tasaki A, Asatani M, Ishikawa H. Quantitative MR texture analysis for the differentiation of uterine smooth muscle tumors with high signal intensity on T2-weighted imaging. Medicine (Baltimore). 2023;102(31):e34452. doi:10.1097/MD.0000000000034452
26. Pati SK, Mondal K, Bodhey NK, Bagde N, Gupta RK, Shukla A. Role of Multiparametric MRI in the Preoperative Evaluation of Endometrial Carcinoma: A Cross-Sectional Study. Cureus. 16(7):e65058. doi:10.7759/cureus.65058
27. Santos P, Cunha TM. Uterine sarcomas: clinical presentation and MRI features. Diagn Interv Radiol. 2015;21(1):4-9. doi:10.5152/dir.2014.14053
28. Kim TH, Kim JW, Kim SY, Kim SH, Cho JY. What MRI features suspect malignant pure mesenchymal uterine tumors rather than uterine leiomyoma with cystic degeneration? J Gynecol Oncol. 2018;29(3):e26. doi:10.3802/jgo.2018.29.e26
29. Himoto Y, Kido A, Sakata A, et al. Differentiation of uterine low-grade endometrial stromal sarcoma from rare leiomyoma variants by magnetic resonance imaging. Sci Rep. 2021;11:19124. doi:10.1038/s41598-021-98473-z
30. Sun S, Bonaffini PA, Nougaret S, et al. How to differentiate uterine leiomyosarcoma from leiomyoma with imaging. Diagnostic and Interventional Imaging. 2019;100(10):619-634. doi:10.1016/j.diii.2019.07.007
31. Jones J. T2-weighted image | Radiology Reference Article | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-6345
32. Charles-Edwards EM, deSouza NM. Diffusion-weighted magnetic resonance imaging and its application to cancer. Cancer Imaging. 2006;6(1):135-143. doi:10.1102/1470-7330.2006.0021
33. Niknejad MT. Apparent diffusion coefficient | Radiology Reference Article | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-21759
34. Gordon Y, Partovi S, Müller-Eschner M, et al. Dynamic contrast-enhanced magnetic resonance imaging: fundamentals and application to the evaluation of the peripheral perfusion. Cardiovasc Diagn Ther. 2014;4(2):147-164. doi:10.3978/j.issn.2223-3652.2014.03.01