Crohn’s disease and ulcerative colitis, two forms of inflammatory bowel disease (IBD), can be debilitating when left untreated. Yet when detected early, individuals can significantly reduce complications, avoid invasive surgeries, and maintain a better quality of life. Early detection not only allows for prompt treatment but also opens the door to non-invasive options like MRI, reducing the burden of frequent colonoscopies. Here’s why catching IBD early truly matters.
Inflammatory bowel disease (IBD) is the long-term, chronic inflammation of the digestive tract caused by an abnormal immune response against the lining of the gut1. Crohn’s disease and ulcerative colitis are the two most common types of IBD; they share multiple symptoms but differ in which part or layer of the gut they affect.
In Crohn’s disease, inflammation can occur anywhere along the length of the gut – from the mouth to the bottom – and can cause inflammation in all layers of the gut. In Colitis, inflammation can occur anywhere in the colon or rectum, and only the inner lining of the gut is affected1.
IBD affects over half a million people in the UK, and an additional 25,000 people are diagnosed with Crohn’s and Colitis each year2,3. However, many experience delays in diagnosis, which can lead to serious complications. This blog will discuss why early detection is so important.
Why Early Detection of Crohn’s and Colitis Is Critical
The early detection of Crohn’s and colitis enables inflammation to be controlled before it leads to damage to the digestive tract.
Slowing Disease Progression
The late diagnosis of IBD puts individuals at greater risk of having already developed more advanced features of the disease at diagnosis. This results in an increasingly complex disease and a greater risk of irreversible complications, making the disease more difficult to treat4.
Treating individuals with IBD early in disease progression enables issues to be resolved before complications arise, leading to remission and reduced bowel damage over time4.
Avoiding Emergency Surgery
Persistent, uncontrolled inflammation in IBD causes significant damage to the digestive tract, including strictures (the abnormal narrowing of the intestines), abscesses, and even cancer5. As a result of these complications, 50 per cent of individuals with Crohn’s and 10 per cent of those with colitis require surgery within 10 years of diagnosis.
Delayed diagnosis puts individuals at a higher risk of surgery, whereas early treatment is thought to decrease the risk of surgery, particularly in Crohn’s disease6–8.
Enhancing Long-Term Health Outcomes
Delays in IBD diagnosis are associated with an increased risk of permanent bowel damage, whereas earlier diagnosis is associated with improved clinical outcomes4,9. Early treatment reduces the risk of complications, surgery, and hospitalisation, enhancing an individual’s quality of life10.
Tools for Early Detection: From Symptoms to Scans
Recognising the Early Signs
The early signs of Crohn’s and colitis are similar but non-specific, meaning that they are often dismissed as stress or irritable bowel syndrome.
Symptoms of Crohn’s include11:
- Diarrhoea
- Blood in the stool
- Stomach or bottom pain
- Fatigue
- Loss of appetite and weight loss
- Slow growth or delayed puberty (specifically in children)
Symptoms of colitis include12:
- Recurring diarrhoea
- Blood, mucus, or pus in the stool
- Tummy pain
- Frequent need to open bowels
- Fatigue
- Loss of appetite and weight loss
Traditional Diagnosis via Endoscopy
Diagnosis of Crohn’s or colitis commonly combines blood tests with more invasive procedures, such as a colonoscopy and biopsy13. Colonoscopies enable medical professionals to directly view the gut lining to identify ulcers and inflammation. During these procedures, they also take biopsies (small pieces of tissue) from the gut. These can be studied under a microscope to differentiate Crohn’s from colitis.
The Role of MRI in Early Diagnosis
Endoscopies, such as colonoscopies, are invasive procedures that are often uncomfortable and can cause mild side effects. While such procedures are necessary for a definitive diagnosis, other procedures can be carried out to complement colonoscopy results or for initial exploration (to avoid patients having to undergo multiple endoscopy procedures).
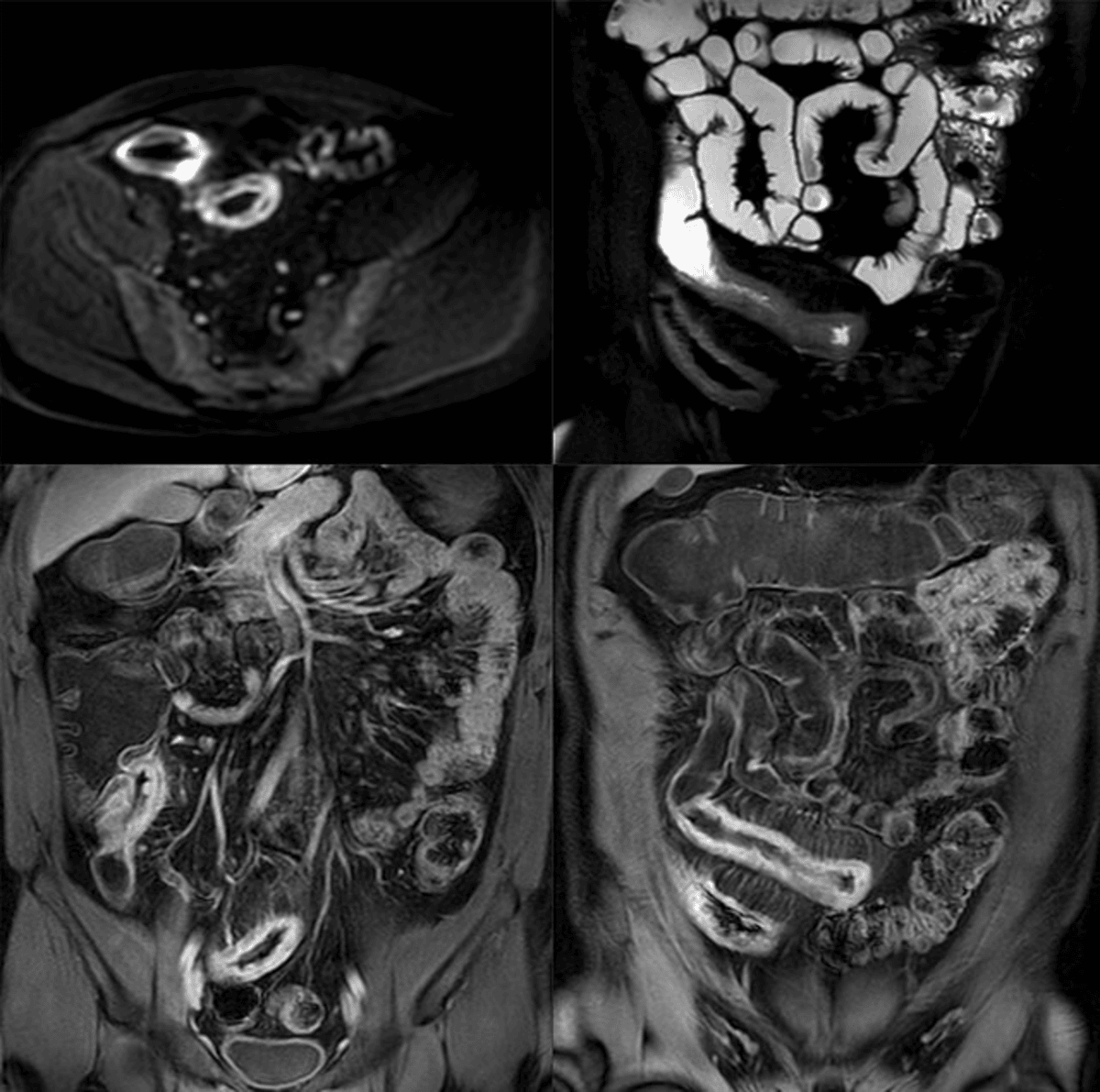
A magnetic resonance imaging enterography (MRE) is a non-invasive way to image the small intestines and bowel. MREs produce highly detailed images, and studies have shown that they show similar accuracy in diagnosing Crohn’s as colonoscopies14. In addition, MREs can obtain images of areas that are difficult to reach via endoscopy.
MREs do not involve exposure to ionizing radiation. As a result, it is safe for individuals to undergo repeat MREs, making them an important tool for the long-term monitoring of Crohn’s or colitis13.
Quality of Life Benefits from Timely Intervention
Managing Symptoms Earlier
The early detection of Crohn’s and colitis enables medication to begin as early as possible in disease progression. Not only does this reduce the risk of complications and hospitalisations, but it also allows individuals to manage debilitating symptoms, leading to disease remission. This drastically improves the quality of life of those living with IBD.
Emotional Well-being and Peace of Mind
The symptoms associated with IBD can be unpleasant and embarrassing, with the potential to lead to mental health problems, such as anxiety and depression. Individuals living with IBD are up to twice as likely to experience mental health problems compared to the general population, leading to a severe impact on quality of life15,16.
Obtaining a diagnosis of IBD can help bring clarity to individuals experiencing IBD symptoms, providing validation and a clearer path forward.
Joining a Crohn’s and colitis community, such as Crohn’s & Colitis UK16, can help individuals with their mental health and provide information on where support can be found.
Life Planning, Fertility, and Family Goals
A diagnosis of IBD and early treatment can help individuals manage their IBD through different life stages. Early treatment enables many individuals to get their condition under control and in remission before planning important life events, such as pregnancy or travel17.
Who Should Consider Early Screening?
Early screening for IBD is recommended for those at an increased risk of developing the disease, including:
- Anyone with a family history of IBD18.
- Anyone experiencing unexplained gastrointestinal symptoms.
- Smokers19.
Yearly MRI screening, where detailed images of at-risk areas are obtained and analyzed for any abnormalities, could be an option for high-risk individuals looking to be proactive about their health. MRIs are non-invasive, making them a key tool for long-term monitoring of health conditions.
Summary
Early detection of Crohn’s and colitis can transform lives by preventing complications and supporting better health from the start. If you’re experiencing unexplained digestive symptoms, don’t wait. Consider speaking with your GP, and take a proactive step by booking an Ezra MRI Scan today. Our annual scan is a fast, non-invasive way to assess your health, leveraging AI through the screening process to make it more efficient and more affordable.
Understand your risk for cancer with our 5 minute quiz.
Our scan is designed to detect potential cancer early.
References
1. All about Crohn’s and Colitis. Accessed December 11, 2025. https://www.crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/understanding-crohns-and-colitis/all-about-crohns-and-colitis
2. IBD UK Report and Press Release. Accessed December 11, 2025. https://www.bsg.org.uk/news/ibd-uk-report-and-press-release
3. New research shows over 1 in 123 people in UK living with Crohn’s or Colitis. Accessed December 11, 2025. https://www.crohnsandcolitis.org.uk/news-stories/news-items/new-research-shows-over-1-in-123-people-in-uk-living-with-crohn-s-or-colitis
4. Danese S, Fiorino G, Fernandes C, Peyrin-Biroulet L. Catching the Therapeutic Window of Opportunity in Early Crohn’s Disease. Current Drug Targets. 2014;15(11):1056-1063.
5. Cantoro L, Monterubbianesi R, Falasco G, et al. The Earlier You Find, the Better You Treat: Red Flags for Early Diagnosis of Inflammatory Bowel Disease. Diagnostics (Basel). 2023;13(20):3183. doi:10.3390/diagnostics13203183
6. Law CCY, Tkachuk B, Lieto S, et al. Early Biologic Treatment Decreases Risk of Surgery in Crohn’s Disease but not in Ulcerative Colitis: Systematic Review and Meta-Analysis. Inflamm Bowel Dis. 2023;30(7):1080-1086. doi:10.1093/ibd/izad149
7. Jayasooriya N, Ballie S, Blackwell J, et al. P630 Systematic review and meta-analysis: Diagnostic delay and the subsequent impact on the disease course of adult Inflammatory Bowel Disease. J Crohns Colitis. 2022;16(Supplement_1):i552. doi:10.1093/ecco-jcc/jjab232.756
8. Lee D won, Koo JS, Choe JW, et al. Diagnostic delay in inflammatory bowel disease increases the risk of intestinal surgery. World J Gastroenterol. 2017;23(35):6474-6481. doi:10.3748/wjg.v23.i35.6474
9. Jayasooriya N, Baillie S, Blackwell J, et al. Systematic review with meta-analysis: Time to diagnosis and the impact of delayed diagnosis on clinical outcomes in inflammatory bowel disease. Alimentary Pharmacology & Therapeutics. 2023;57(6):635-652. doi:10.1111/apt.17370
10. Jayasooriya N, Saxena S, Blackwell J, et al. Associations between prior healthcare use, time to diagnosis, and clinical outcomes in inflammatory bowel disease: a nationally representative population-based cohort study. BMJ Open Gastroenterol. 2024;11(1). doi:10.1136/bmjgast-2024-001371
11. Crohn’s disease. nhs.uk. October 23, 2017. Accessed December 11, 2025. https://nhsuk-cms-fde-prod-uks-dybwftgwcqgsdmfh.a03.azurefd.net/conditions/crohns-disease/
12. Ulcerative colitis. nhs.uk. October 3, 2018. Accessed December 11, 2025. https://nhsuk-cms-fde-prod-uks-dybwftgwcqgsdmfh.a03.azurefd.net/conditions/ulcerative-colitis/
13. Hong SM, Baek DH. Diagnostic Procedures for Inflammatory Bowel Disease: Laboratory, Endoscopy, Pathology, Imaging, and Beyond. Diagnostics (Basel). 2024;14(13):1384. doi:10.3390/diagnostics14131384
14. Grand DJ, Kampalath V, Harris A, et al. MR enterography correlates highly with colonoscopy and histology for both distal ileal and colonic Crohn’s disease in 310 patients. European Journal of Radiology. 2012;81(5):e763-e769. doi:10.1016/j.ejrad.2012.02.011
15. Mitropoulou MA, Fradelos EC, Lee KY, et al. Quality of Life in Patients With Inflammatory Bowel Disease: Importance of Psychological Symptoms. Cureus. 14(8):e28502. doi:10.7759/cureus.28502
16. Mental health and wellbeing with Crohn’s or Colitis. Accessed December 11, 2025. https://www.crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/living-with-crohns-or-colitis/mental-health-and-wellbeing
17. Pregnancy and breastfeeding with Crohn’s Disease or Ulcerative Colitis (IBD). Accessed December 11, 2025. https://www.crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/living-with-crohns-or-colitis/pregnancy-and-breastfeeding
18. Santos MPC, Gomes C, Torres J. Familial and ethnic risk in inflammatory bowel disease. Ann Gastroenterol. 2018;31(1):14-23. doi:10.20524/aog.2017.0208
19. Chhibba T, Gros B, King JA, et al. Environmental risk factors of inflammatory bowel disease: toward a strategy of preventative health. J Crohns Colitis. 2025;19(4):jjaf042. doi:10.1093/ecco-jcc/jjaf042