The spine is made up of 33 vertebrae, seven of which make up the cervical, or neck area (C1 - C7)1. It also contains and protects the spinal cord, which functions as a complex bundle of nervous cells that help send and receive signals to and from the rest of our body.
MRI is especially valuable for detecting early-stage cancer in the cervical spine. MRI can detect subtle changes in bone marrow, showing tumour infiltration before it becomes visible on other imaging tests2. Faint abnormalities in the spinal cord, such as T2 signal changes, can be detected before X-ray or CT, allowing for earlier intervention and more effective treatment planning3.
When interpreting a cervical spine MRI, three key checks are conducted:
Learn more about MRI for cancer detection here.
There are several reasons why a cervical spine MRI might be ordered, including:
Evaluate your cancer risk with our 5-minute quiz.
Here are a few tips to help you prepare for your MRI16:
You can read more about preparation for Ezra’s Full Body Scan here.
Upon arrival for your MRI, you will need to check in and complete a screening form. This will allow you to confirm the presence of implants, allergies, and whether you might need any anxiety medication.
During the MRI, you’ll lie on your back with your head and neck positioned in a special coil that helps capture high-quality images17. The scan typically covers from the base of your skull (C0) down to the upper thoracic spine (T2), ensuring that no important region is missed.
The technologist will acquire several sets of images, known as sequences, each designed to highlight different tissues and problems. High-resolution sagittal views allow precise measurement of disc height at every level and can reveal changes in disc signal intensity, which may indicate degeneration or injury18.
You’ll hear a series of loud knocking or tapping sounds as the MRI machine works. This is completely normal. The scan usually takes about 20 to 45 minutes, and you’ll be offered earplugs or headphones to make the experience more comfortable.
The different sequences, such as T1, T2, short tau inversion recovery (STIR), and sometimes post-contrast images, can reveal subtle abnormalities, such as cavities within the spinal cord (syringomyelia) or areas where the spinal canal has collapsed19. These detailed images help doctors identify issues such as nerve compression, disc herniation, tumours, or post-surgical changes, all in a single scan.
You’ll stay in touch with the team via a two-way intercom and a squeeze bulb, allowing you to communicate or pause the scan if needed. If contrast is required, it’s injected halfway through, possibly causing a brief cool sensation. After the final sequence, the coil is removed, and you’re free to go.
At Ezra, our Full Body Plus scan takes around 60 minutes total, with 45 minutes of table time. Earplugs or headphones are available.
MRI is generally considered very safe when proper screening and protocols are followed, but certain risks and side effects should be understood:
A deeper dive into possible side effects (such as heat, headaches, and gadolinium deposition) is available in our full guide.
At Ezra, we employ a contrast-free approach using wide-bore T3 machines to deliver a comfortable scanning experience.
There are a number of terms you might see in your MRI report after your cervical spine scan. Here are some explanations for some common ones:
Ezra provides a radiologist-reviewed report in a non-technical and easy-to-understand format on your dashboard34.
After the MRI scan, you will be free to go home and continue with your day without any precautions35. If you received a sedative, you will need another person to pick you up. You will also not be able to drive, consume alcohol or operate heavy machinery 24 hours after the sedative.
A team of experts will review your results and determine whether a follow-up is necessary and recommend the appropriate treatment if needed. If abnormalities are found, you may undergo ongoing monitoring every 2-3 months to track recurrence. You can receive support in the form of counselling and advice on how to handle aspects like claustrophobia.
If you have a scan with us here at Ezra, you will receive your report within five to seven days and have the option to discuss it with a medical practitioner. You can also access your scan images through the online portal.
MRI is a powerful tool for detecting and evaluating cervical spine cancer, often revealing abnormalities long before other imaging methods.
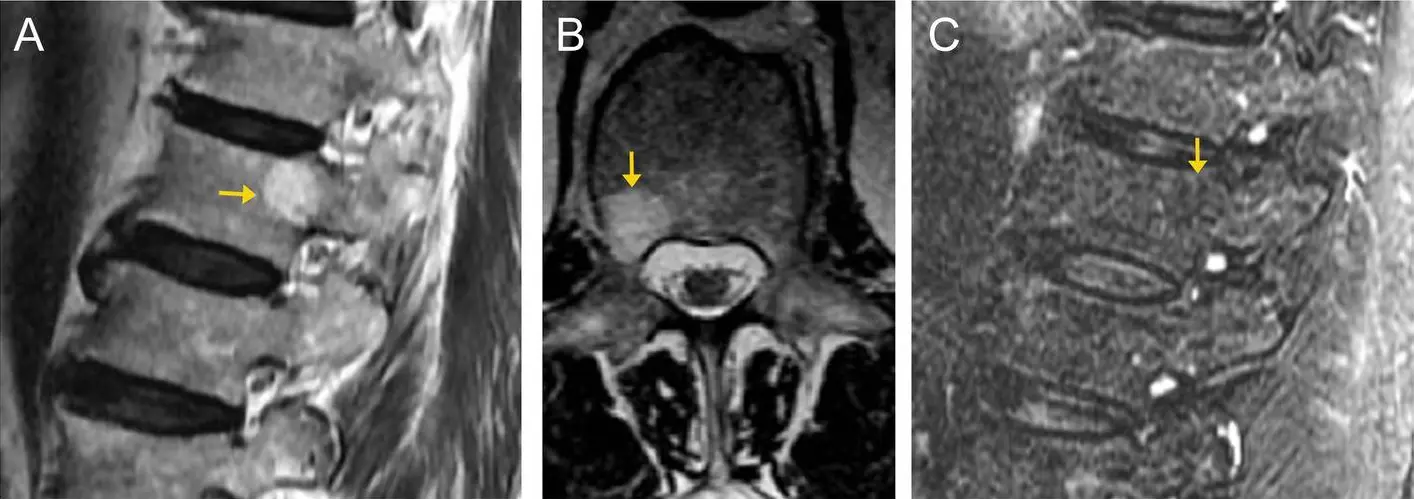
MRI can detect subtle changes in the bone marrow within the vertebrae at an early stage, well before these changes are visible on X-ray or CT scans. These early alterations, such as decreased signal intensity on T1-weighted images and increased signal on STIR sequences, may indicate tumour infiltration or marrow swelling (oedema), providing a critical head start for diagnosis and treatment planning36,37.
MRI excels at mapping the precise extent of a tumour, including its infiltration into bone, the epidural space, or surrounding soft tissues38. It can show whether a tumour has breached the vertebral body, invaded the spinal canal, or extended into paraspinal tissues. This level of detail is essential for surgical planning and assessing the risk of spinal cord compression or instability39.
One of the key indirect signs of cancer-related damage on MRI is a bright signal within the spinal cord on T2-weighted images40,41. This T2 hyperintensity often signals early myelopathy, indicating that the spinal cord is under pressure or has suffered injury, even before severe symptoms develop. Such findings can prompt urgent intervention to prevent permanent neurological deficits.
MRI is also highly sensitive to swelling of the paraspinal soft tissues and can detect compression of the spinal canal by bone spurs, tumour mass, or inflamed tissues38,39. These changes may not be apparent on other imaging modalities but are crucial for diagnosing the cause of pain, neurological symptoms, or impending spinal cord compromise.
Ezra utilises DWI as part of our whole-body MRI scans and artificial intelligence (AI) to enhance MRI images and convert radiology reports into layman's term translations.
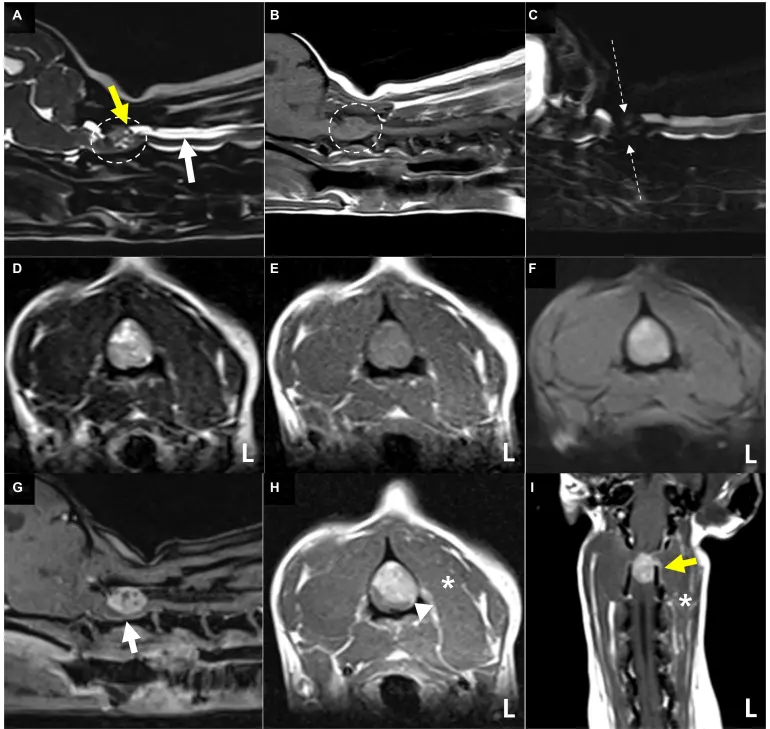
Primary Bone Tumours (Chordoma, Osteosarcoma) and Lymphoma-like Lesions: Chordoma tumours appear as a loculated mass with high T2 signal, often with an extra-osseous soft tissue component. They may show areas of high T1 signal, due to haemorrhage or calcification47. Osteosarcoma shows low T1 and variable T2 signal with extra-osseous extension; mineralisation may appear as low T2 signal foci48. Lymphomas typically present as a mass replacing marrow, with low to intermediate T1 signal and increased signal on fluid-sensitive sequences (T2/STIR), often with soft-tissue extension.
Vertebral Artery Anomaly at C1-C2: Any vertebral artery anomaly in the upper cervical region (C1-C2) is critical to identify before surgery, as it may complicate tumour resection or stabilisation procedures49. MRI and MR angiography can help flag such anomalies for surgical planning.
Ezra screens for over 500 conditions and 13 organs, including the spine.
There are multiple types of MRI scans, all using different methods to give a better visualisation of cervical spine tumours.
Ezra’s MRI Scan with Spine costs £2,395 and is currently available at their partner clinic in Marylebone, London and Sidcup, with more locations planned in the future.
No referral is required, so you can book your scan directly without first consulting a GP or specialist.
Most people pay out-of-pocket, as insurance typically does not cover self-referred scans, but you may be able to seek reimbursement depending on your policy.
A cervical spine MRI is a non-invasive scan that uses magnetic fields to create detailed images of the neck’s bones, discs, spinal cord, and surrounding tissues.
A cervical MRI focuses on the neck region, but the upper parts of the shoulders may appear at the edges of the images.
Yes, an MRI of the neck can detect tumours, cancer spread, and related changes in the cervical spine or surrounding soft tissues.
It shows the vertebrae, discs, spinal cord, nerve roots, ligaments, and nearby soft tissues, helping to identify injuries, degeneration, or disease.
No, typically only your head and upper shoulders enter the scanner for a cervical spine MRI.
A cervical MRI may show the lower part of the brainstem and cerebellum, but it is not designed to image the entire brain.
Doctors order a cervical spine MRI to investigate persistent neck pain, nerve symptoms, trauma, suspected cancer, or post-surgical complications.
Ready to take proactive steps for your health? Book an Ezra full-body MRI today to detect any issues early and put you on the road to long-term health. Our yearly scan screens for potential cancers early, using AI to enhance the process, making it more efficient and affordable.



1. Kaiser JT, Reddy V, Launico MV, et al. Anatomy, Head and Neck: Cervical Vertebrae. In: StatPearls. StatPearls Publishing; 2025. Accessed July 9, 2025. http://www.ncbi.nlm.nih.gov/books/NBK539734/
2. Zhong X, Li L, Lu B, et al. Differentiation of Cervical Spine Osteoradionecrosis and Bone Metastasis After Radiotherapy Detected by Bone Scan in Patients With Nasopharyngeal Carcinoma: Role of Magnetic Resonance Imaging. Front Oncol. 2020;10:15. doi:10.3389/fonc.2020.00015
3. Mascalchi M, Vella A. Neuroimaging Applications in Chronic Ataxias. Int Rev Neurobiol. 2018;143:109-162. doi:10.1016/bs.irn.2018.09.011
4. Sarotto AJ, Rosado Pardo J, Fossa Riglos S, et al. Cervical pedicle agenesis: case report and bibliographic review. Surg Radiol Anat. 2020;42(2):121-125. doi:10.1007/s00276-019-02333-5
5. Karabag H, Iplikcioglu AC. Upper and lower cervical alignment parameters measured on supine magnetic resonance imaging with the occipital slope as a key marker of cervical alignment. J Craniovertebr Junction Spine. 2024;15(1):61-65. doi:10.4103/jcvjs.jcvjs_185_23
6. Li AY, McCarthy L, Hrabarchuk E, et al. Novel Grading Scales for Static and Flexion-Extension Magnetic Resonance Imaging in Patients with Cervical Spondylotic Myelopathy. World Neurosurg. 2023;173:e218-e227. doi:10.1016/j.wneu.2023.02.034
7. Redebrandt HN, Brandt C, Hawran S, et al. Clinical evaluation versus magnetic resonance imaging findings in patients with radicular arm pain—A pragmatic study. Health Sci Rep. 2022;5(3):e589. doi:10.1002/hsr2.589
8. Kang KC, Lee HS, Lee JH. Cervical Radiculopathy Focus on Characteristics and Differential Diagnosis. Asian Spine J. 2020;14(6):921-930. doi:10.31616/asj.2020.0647
9. Tsuchiya K, Honya K, Yoshida M, et al. Demonstration of spinal cord and nerve root abnormalities by diffusion neurography. J Comput Assist Tomogr. 2008;32(2):286-290. doi:10.1097/RCT.0b013e31814625e3
10. National Institute for Health and Care Excellence. Spinal metastases and metastatic spinal cord compression. Published online 2023. Accessed July 9, 2025. https://www.nice.org.uk/guidance/ng234/evidence/d-recognition-spinal-metastases-pdf-13134698176
11. Montoya-Bordón J, Elvira-Ruiz P, Carriazo-Jiménez B, et al. Imaging diagnosis of vertebral metastasis. Revista Española de Cirugía Ortopédica y Traumatología. 2023;67(6):S511-S522. doi:10.1016/j.recot.2023.08.006
12. Guimaraes MD, Bitencourt AG, Marchiori E, et al. Imaging acute complications in cancer patients: what should be evaluated in the emergency setting? Cancer Imaging. 2014;14(1):18. doi:10.1186/1470-7330-14-18
13. Byvaltsev VA, Kalinin AA, Aliyev MA, et al. Postoperative MRI Visualization of the Cervical Spine Following Cervical Disc Arthroplasty: A Prospective Single-Center Comparison of a Titanium and Cobalt-Chromium Prosthesis. Global Spine J. 2023;13(1):67-73. doi:10.1177/2192568221991105
14. Daskareh M, Esmaeilian S, Rahmanipour E, et al. Evaluating the pivotal role of MRI in craniocervical junction injury diagnosis: A case report. Medicine (Baltimore). 2025;104(21):e42154. doi:10.1097/MD.0000000000042154
15. Riascos R, Bonfante E, Cotes C, et al. Imaging of Atlanto-Occipital and Atlantoaxial Traumatic Injuries: What the Radiologist Needs to Know. RadioGraphics. 2015;35(7):2121-2134. doi:10.1148/rg.2015150035
16. Radiology (ACR) RS of NA (RSNA) and AC of. Magnetic Resonance Imaging (MRI) - Head. Radiologyinfo.org. Accessed July 3, 2025. https://www.radiologyinfo.org/en/info/mri-brain
17. MRI scans. Newcastle Hospitals NHS Foundation Trust. February 10, 2021. Accessed July 9, 2025. https://www.newcastle-hospitals.nhs.uk/services/radiology/mri-scans/
18. Thompson J, Brismée JM, Page P, et al. Validity & Reliability of Using Musculoskeletal Ultrasound to Measure Cervical Disc Height. Int J Sports Phys Ther. 20(7):964-973. doi:10.26603/001c.140889
19. Alcaide-Leon P, Pauranik A, Alshafai L, et al. Comparison of Sagittal FSE T2, STIR, and T1-Weighted Phase-Sensitive Inversion Recovery in the Detection of Spinal Cord Lesions in MS at 3T. AJNR Am J Neuroradiol. 2016;37(5):970-975. doi:10.3174/ajnr.A4656
20. Gill A, Shellock FG. Assessment of MRI issues at 3-Tesla for metallic surgical implants: findings applied to 61 additional skin closure staples and vessel ligation clips. J Cardiovasc Magn Reson. 2012;14(1):3. doi:10.1186/1532-429X-14-3
21. Potential Hazards and Risks. UCSF Radiology. January 20, 2016. Accessed March 14, 2025. https://radiology.ucsf.edu/patient-care/patient-safety/mri/potential-hazards-risks
22. Costello JR, Kalb B, Martin DR. Incidence and Risk Factors for Gadolinium-Based Contrast Agent Immediate Reactions. Top Magn Reson Imaging. 2016;25(6):257-263. doi:10.1097/RMR.0000000000000109
23. McDonald RJ, McDonald JS, Kallmes DF, et al. Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017;285(2):546-554. doi:10.1148/radiol.2017161595
24. Keskin NK, Yurtluk MD, Başdemirci M, et al. EVALUATING INCIDENTAL FINDINGS IN CERVICAL MRI SCANS: THE PREVALENCE AND CLINICAL RELEVANCE OF INCIDENTAL FINDINGS. The Journal of Turkish Spinal Surgery. Published online January 22, 2025. doi:10.4274/jtss.galenos.2024.73792
25. Mall MA, Stahl M, Graeber SY, et al. Early detection and sensitive monitoring of CF lung disease: Prospects of improved and safer imaging. Pediatr Pulmonol. 2016;51(S44):S49-S60. doi:10.1002/ppul.23537
26. Raja A, Patel P, Mesfin FB. Spinal Stenosis. In: StatPearls. StatPearls Publishing; 2025. Accessed July 9, 2025. http://www.ncbi.nlm.nih.gov/books/NBK441989/
27. Park CH, Lee SH. Effectiveness of percutaneous transforaminal adhesiolysis in patients with lumbar neuroforaminal spinal stenosis. Pain Physician. 2013;16(1):E37-43.
28. Myelomalacia - an overview | ScienceDirect Topics. Accessed July 9, 2025. https://www.sciencedirect.com/topics/medicine-and-dentistry/myelomalacia
29. Syringomyelia - Support for neurological conditions | The Brain Charity. Accessed July 9, 2025. https://www.thebraincharity.org.uk/condition/syringomyelia/
30. Viswanathan VK, Shetty AP, Rajasekaran S. Modic changes - An evidence-based, narrative review on its patho-physiology, clinical significance and role in chronic low back pain. J Clin Orthop Trauma. 2020;11(5):761-769. doi:10.1016/j.jcot.2020.06.025
31. Facet Joint Arthritis London, UK | Osteophytes London | Spine Arthritis. Accessed July 9, 2025. https://www.londonspinecare.co.uk/facet-joint-arthritis-trauma-orthopaedic-surgeon-london.html
32. Aryal V, Black AC, Jimenez A. Anatomy, Back, Posterior Longitudinal Ligament. In: StatPearls. StatPearls Publishing; 2025. Accessed July 9, 2025. http://www.ncbi.nlm.nih.gov/books/NBK560691/
33. Counterpoint: Appropriately Ambiguous—The Disc Osteophyte Complex. AJNR Am J Neuroradiol. 2016;37(12):2181. doi:10.3174/ajnr.A4928
34. Zampa V, Roselli G, Beltrami G. MRI of bone tumors: advances in diagnosis and treatment assessment. Imaging in Medicine. 2010;2(3):325–340.
35. MRI scan. NHS inform. Accessed July 3, 2025. https://www.nhsinform.scot/tests-and-treatments/scans-and-x-rays/mri-scan/
36. Ollivier L, Gerber S, Vanel D, et al. Improving the interpretation of bone marrow imaging in cancer patients. Cancer Imaging. 2006;6(1):194-198. doi:10.1102/1470-7330.2006.0034
37. Grønningsæter IS, Ahmed AB, Vetti N, et al. Bone marrow abnormalities detected by magnetic resonance imaging as initial sign of hematologic malignancies. Clin Pract. 2018;8(2):1061. doi:10.4081/cp.2018.1061
38. MacVicar D. Imaging of the spine in patients with malignancy. Cancer Imaging. 2006;6(Spec No A):S22-S26. doi:10.1102/1470-7330.2006.9002
39. Creze M, Ghaouche J, Missenard G, et al. Understanding a mass in the paraspinal region: an anatomical approach. Insights Imaging. 2023;14:128. doi:10.1186/s13244-023-01462-1
40. Grayev AM, Kissane J, Kanekar S. Imaging approach to the cord T2 hyperintensity (myelopathy). Radiol Clin North Am. 2014;52(2):427-446. doi:10.1016/j.rcl.2013.11.002
41. Lee MJ, Aronberg R, Manganaro MS, et al. Diagnostic Approach to Intrinsic Abnormality of Spinal Cord Signal Intensity. RadioGraphics. 2019;39(6):1824-1839. doi:10.1148/rg.2019190021
42. Nguyen TT, Thelen JC, Bhatt AA. Bone up on spinal osseous lesions: a case review series. Insights Imaging. 2020;11:80. doi:10.1186/s13244-020-00883-6
43. Song KW, Shin SI, Lee JY, et al. Surgical Results of Intradural Extramedullary Tumors. Clin Orthop Surg. 2009;1(2):74-80. doi:10.4055/cios.2009.1.2.74
44. Arnautovic K, Arnautovic A. EXTRAMEDULLARY INTRADURAL SPINAL TUMORS: A REVIEW OF MODERN DIAGNOSTIC AND TREATMENT OPTIONS AND A REPORT OF A SERIES. Bosn J Basic Med Sci. 2009;9(Suppl 1):S40-S45. doi:10.17305/bjbms.2009.2755
45. Davidson CL, Das JM, Mesfin FB. Intramedullary Spinal Cord Tumors. In: StatPearls. StatPearls Publishing; 2025. Accessed July 9, 2025. http://www.ncbi.nlm.nih.gov/books/NBK442031/
46. Kim J, Kim K, Chung DJ, et al. Case report: Magnetic resonance imaging features with postoperative improvement of atypical cervical glioma characterized by predominant extramedullary distribution in a dog. Front Vet Sci. 2024;11. doi:10.3389/fvets.2024.1400139
47. Smolders D, Wang X, Drevelengas A, et al. Value of MRI in the diagnosis of non-clival, non-sacral chordoma. Skeletal Radiol. 2003;32(6):343-350. doi:10.1007/s00256-003-0633-1
48. Ariyaratne S, Jenko N, Iyengar KP, et al. Primary Osseous Malignancies of the Spine. Diagnostics (Basel). 2023;13(10):1801. doi:10.3390/diagnostics13101801
49. Rathakrishnan RKV, Raghavendra SK. Managing the Anomalous Vertebral Artery in C1–C2 Stabilization for Congenital Atlantoaxial Instability. J Neurol Surg B Skull Base. 2021;82(Suppl 1):S63-S64. doi:10.1055/s-0040-1714404
50. de Paiva JLR, Sabino JV, Pereira FV, et al. The Role of MRI in the Diagnosis of Spinal Cord Tumors. Seminars in Ultrasound, CT and MRI. 2023;44(5):436-451. doi:10.1053/j.sult.2023.03.012
51. Ghanem NA, Pache G, Lohrmann C, et al. MRI and 18FDG-PET in the assessment of bone marrow infiltration of the spine in cancer patients. Eur Spine J. 2007;16(11):1907-1912. doi:10.1007/s00586-007-0350-x
52. Johnson AJ, Ying J, Gammal TE, et al. Which MR Imaging Sequences Are Necessary in Determining the Need for Radiation Therapy for Cord Compression? A Prospective Study. AJNR: American Journal of Neuroradiology. 2007;28(1):32.
53. Dörflinger-Hejlek E, Kirsch EC, Reiter H, et al. Diffusion-Weighted MR Imaging of Intramedullary Spinal Cord Abscess. AJNR Am J Neuroradiol. 2010;31(9):1651-1652. doi:10.3174/ajnr.A1912
54. Xiao L, Siu CWJ, Yeung K, et al. MRI of the cervical spine with 3D gradient echo sequence at 3 T: initial experience. Clin Radiol. 2015;70(9):926-931. doi:10.1016/j.crad.2015.05.012